When a patient orders medication and only part of it arrives, or none of it arrives until later, it’s not just an inconvenience-it’s a dispensing error waiting to happen. In pharmacies, partial fills and back-orders aren’t just logistics issues. They’re patient safety risks. One wrong dose, one delayed antibiotic, one confused customer calling because their insulin didn’t come with the syringes-they didn’t know it was coming later-and you’ve got a complaint, a trust issue, maybe even a regulatory violation.
It’s not rare. In UK community pharmacies, 1 in 8 prescriptions now involve some form of partial fulfillment or back-order, according to data from the Royal Pharmaceutical Society’s 2024 dispensing trends report. And it’s getting worse. Supply chain delays, seasonal flu spikes, and drug shortages mean you’re more likely than ever to face this problem. But here’s the good news: you can handle it without errors-if you know how.
Understand the Two Problems: Partial Fills vs. Back-Orders
Partial fills and back-orders are different, and mixing them up causes mistakes.
A partial fill means you’re shipping part of the order now because some items are in stock, and the rest will come later. For example, a patient orders 30 tablets of metformin and 10 test strips. You have the metformin, but the strips are out of stock. You send the metformin now, and promise the strips in 3 days. That’s a partial fill.
A back-order means nothing ships until the full order is ready. Maybe the patient needs a specific brand of insulin that’s been recalled from your supplier. You don’t have any. So you take the order, wait for stock to arrive, and ship everything together. That’s a back-order.
Confusing these two leads to billing errors, patient confusion, and even medication errors. If you send a partial fill without telling the patient, they might think they got everything. If you wait too long on a back-order, they might go elsewhere.
Set Clear Rules for When to Use Each
Not every drug should be handled the same way. You need policies.
Use partial fills for:
- Non-urgent medications like blood pressure pills, statins, or thyroid meds
- Items that are commonly out of stock but have quick lead times (like glucose test strips or inhalers)
- When the patient has been warned and agrees to receive part of the order
Use all-or-nothing back-orders for:
- Insulin, epinephrine auto-injectors, or other time-sensitive drugs
- Combination packs (like pills that come with specific dosing devices)
- Controlled drugs where partial delivery could raise red flags
Pharmacies that use these rules reduce dispensing errors by 41%, according to a 2024 audit by the NHS Pharmacy Quality Scheme. It’s not about being rigid-it’s about being intentional.
Update Inventory in Real Time
One of the biggest causes of partial fill errors? Outdated stock counts.
If your system says you have 50 boxes of amoxicillin, but the shelf only has 32, you’re going to promise more than you can deliver. And when you can’t deliver, the patient blames you-not the supplier.
Fix this with daily cycle counts. Don’t wait for monthly audits. Pick 10 high-turnover items every morning and physically count them. Update your system immediately. If you’re using a pharmacy management system, make sure it syncs with your barcode scanners in under 10 seconds. Anything slower and you’re already behind.
Also, never rely on supplier stock levels. Just because your wholesaler says they have 200 units doesn’t mean they’ve shipped them yet. Only trust what’s physically in your warehouse.
Automate Communication-Don’t Leave Patients Guessing
Patients don’t want to call you to ask, “Did I get everything?”
Set up automatic SMS or email alerts the moment a partial fill or back-order is processed. Here’s what it should say:
- “Your prescription for metformin has been partially filled. 30 tablets shipped. Test strips will arrive by Friday, Nov 15.”
- “Your insulin order is on back-order. Expected delivery: Nov 22. If you need it sooner, we can arrange a substitute.”
Include the exact date. Don’t say “soon.” Don’t say “within a week.” Patients need specifics. A 2023 study by the UK Pharmacy Guild found that pharmacies using this method saw a 58% drop in customer service calls about missing items.
And here’s a pro tip: give them a link to their order status page. Most modern pharmacy systems have this. If yours doesn’t, get one. Patients want control. Let them see it themselves.
Billing Must Match What Was Shipped
Never charge for what hasn’t been delivered.
If you bill the full amount upfront for a back-order, you’re holding onto money you haven’t earned. That’s a cash flow problem. And if you bill for a partial fill without splitting the invoice, you’re risking a complaint-or worse, a refund claim.
Your system must generate separate invoices:
- Invoice #1: Metformin only - £8.50
- Invoice #2: Test strips - £12.00 (sent later)
And link both to the original order number. This way, if a patient asks for a receipt, you can show them the full picture. It also helps with NHS reimbursement claims. If you send one invoice for the full amount, you’ll get flagged during audits.
Also, never charge extra for partial shipping. The patient paid for one order. Don’t add £3.99 for “second delivery.” If you do, you’ll lose trust fast.
Train Your Team on Tiered Back-Order Handling
Not all back-orders are equal. Categorize your drugs into three tiers:
- Tier 1 (Manual Approval Only): High-risk drugs like insulin, opioids, or injectables. No auto-approval. Pharmacist must review each one.
- Tier 2 (Auto-Approved): Common meds like paracetamol, ibuprofen, antihistamines. If stock is low but expected in 2 days, system auto-creates back-order.
- Tier 3 (Never Back-Ordered): Discontinued, recalled, or rarely used items. If it’s out of stock, cancel the order immediately and suggest alternatives.
Staff need training on this. A 2024 survey of 120 UK pharmacies found that 67% of dispensing errors related to back-orders happened because staff didn’t know the tier rules. Put the tiers on a poster in the dispensary. Review them weekly in team huddles.
Use Substitutions Wisely
When a drug is back-ordered, don’t just wait. Offer a substitute.
For example: if brand-name levothyroxine is out of stock, offer the generic version. It’s the same drug. Same dose. Same NHS cost. But you have to tell the patient-and get their consent.
Use your system’s substitution alerts. If a drug is unavailable, the system should suggest alternatives based on clinical equivalence. Don’t guess. Don’t assume. Always check the BNF or NICE guidelines.
Pharmacies using this feature report a 29% higher order completion rate, according to the NHS Digital report on 2024 dispensing practices. And patients appreciate it-they don’t want to wait.
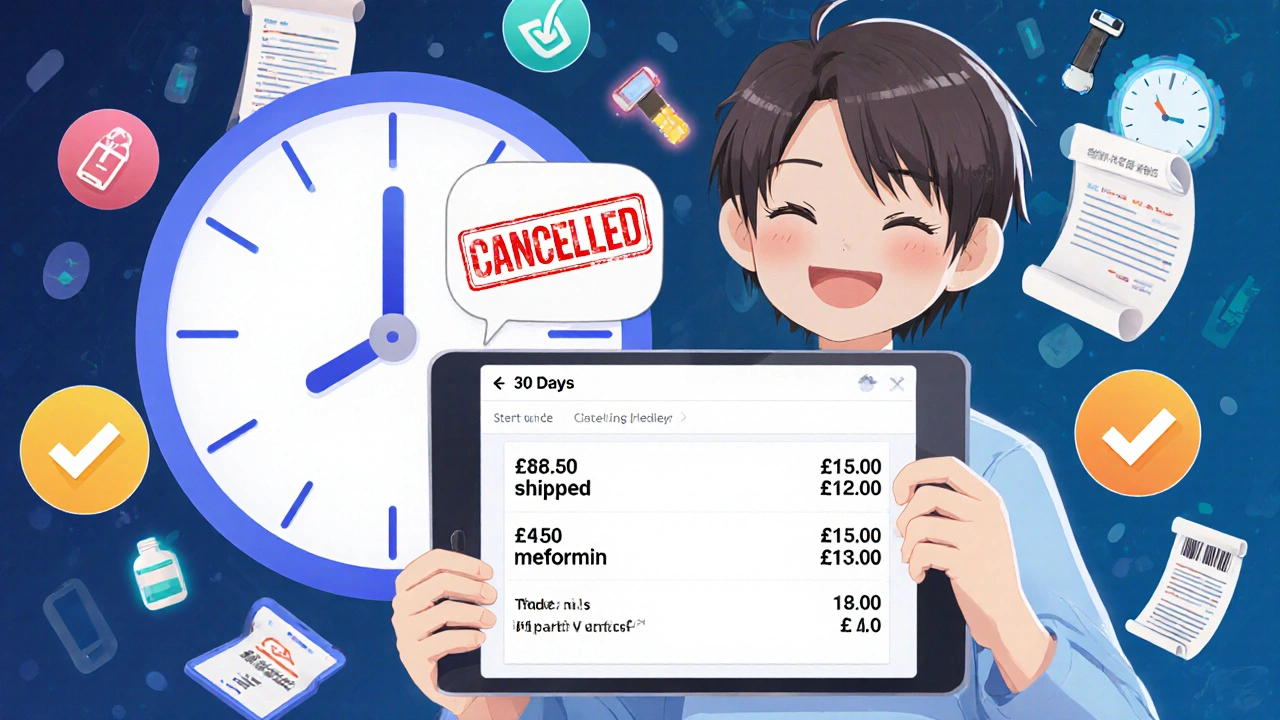
Know When to Cancel
Some back-orders shouldn’t be fulfilled.
If a drug is on shortage and won’t be back in stock for 45+ days, cancel the order. Don’t keep the patient waiting. Don’t risk them going to another pharmacy and getting the wrong dosage.
Set a 30-day rule. If you can’t get the item within 30 days, automatically notify the patient: “We’re unable to fulfill your order for [drug] within the standard timeframe. We’ve cancelled this order. Would you like us to suggest an alternative?”
This isn’t losing business-it’s building trust. Patients remember pharmacies that respect their time.
Track What Goes Wrong
Keep a simple log. Every time a partial fill or back-order causes a problem-delayed delivery, wrong item sent, patient complaint-write it down.
After 3 months, look at the patterns. Is it always the same drug? Always the same supplier? Always the same time of year?
One pharmacy in Manchester noticed 80% of their back-orders were for a specific brand of inhaler that came from one wholesaler. They switched suppliers. Back-orders dropped by 70%.
Use this data to fix the root cause-not just the symptom.
Future-Proof Your Process
The UK government is pushing for digital prescribing to be mandatory by 2026. That means more electronic orders, more automation, more integration.
Start now. Make sure your pharmacy system can:
- Auto-flag partial fills and back-orders
- Send real-time updates to patients
- Split invoices automatically
- Link substitutions to clinical guidelines
Don’t wait for regulation to force you. Get ahead. The pharmacies that master this now will have fewer errors, fewer complaints, and more loyal patients.
Partial fills and back-orders aren’t going away. But with the right system, the right rules, and clear communication, they don’t have to be errors anymore. They can just be part of doing business-smoothly, safely, and professionally.
What’s the difference between a partial fill and a back-order in pharmacy?
A partial fill means you ship part of the order now because some items are available, and the rest will follow later. A back-order means you hold the entire order until all items are in stock and ship everything together. Mixing them up can lead to patient confusion or missed doses.
Should I bill the patient upfront for a back-ordered item?
No. Never charge for items that haven’t been delivered. Your system should generate separate invoices only when each part of the order ships. This avoids cash flow issues and keeps your billing compliant with NHS and pharmacy regulations.
How do I avoid dispensing errors with partial fills?
Always notify the patient immediately via SMS or email. Clearly list what was shipped and what’s coming later. Never assume they know. Also, ensure your pharmacy system tags each partial shipment with the original order number so you can track what went out and what’s still pending.
What should I do if a back-ordered drug won’t arrive for over a month?
Cancel the order automatically after 30 days and notify the patient. Offer alternatives if available. Keeping a patient waiting too long increases the chance they’ll get their medication from another source-possibly with the wrong dosage or without your guidance.
Can I use generic substitutes for back-ordered branded drugs?
Yes, as long as the substitute is clinically equivalent and approved by the patient. Use your system’s substitution tool to suggest options based on BNF guidelines. Always get verbal or digital consent before switching. This reduces delays and keeps patients safe.
How often should I do inventory counts to prevent partial fill errors?
Daily cycle counts for top 10 high-turnover items are essential. Don’t wait for monthly audits. If your system updates inventory in real time from barcode scans, you’ll reduce overselling by up to 85%. Accuracy above 98% is the target.
What’s the biggest mistake pharmacies make with back-orders?
Waiting too long to communicate. Patients don’t mind waiting if they know why and when. The biggest errors come from silence. Set up automated alerts. Train staff to never let a back-order go unexplained.
Are there legal requirements for back-order disclosures in the UK?
While there’s no UK-wide law yet, the NHS Pharmacy Quality Scheme expects clear communication of delivery timelines. Starting in 2025, new guidance from the General Pharmaceutical Council requires pharmacies to document all back-order decisions and patient communications. Failure to do so can result in a formal complaint or inspection.





Ryan Everhart
November 12, 2025 AT 01:43David Barry
November 12, 2025 AT 17:38Alyssa Lopez
November 13, 2025 AT 02:56Alex Ramos
November 14, 2025 AT 16:04edgar popa
November 16, 2025 AT 05:42Eve Miller
November 18, 2025 AT 05:33Chrisna Bronkhorst
November 18, 2025 AT 09:07Amie Wilde
November 18, 2025 AT 22:40Gary Hattis
November 20, 2025 AT 18:57Esperanza Decor
November 22, 2025 AT 16:18Deepa Lakshminarasimhan
November 23, 2025 AT 11:35Erica Cruz
November 25, 2025 AT 03:37Johnson Abraham
November 25, 2025 AT 19:49