The Pharmaceutical Benefits Scheme (PBS) is the backbone of Australia’s public healthcare system when it comes to prescription drugs. It’s not just a subsidy program-it’s the reason millions of Australians can afford life-saving medications without going broke. Since 1948, the PBS has ensured that essential medicines are available at low cost to anyone with a Medicare card. Today, it covers over 5,400 drugs, and nearly 87% of all prescriptions in Australia are subsidized through it. But behind the numbers is a complex, high-stakes system that shapes how generics enter the market, who gets access, and how much the government-and patients-pay.
How the PBS Works: Subsidies, Co-Payments, and Safety Nets
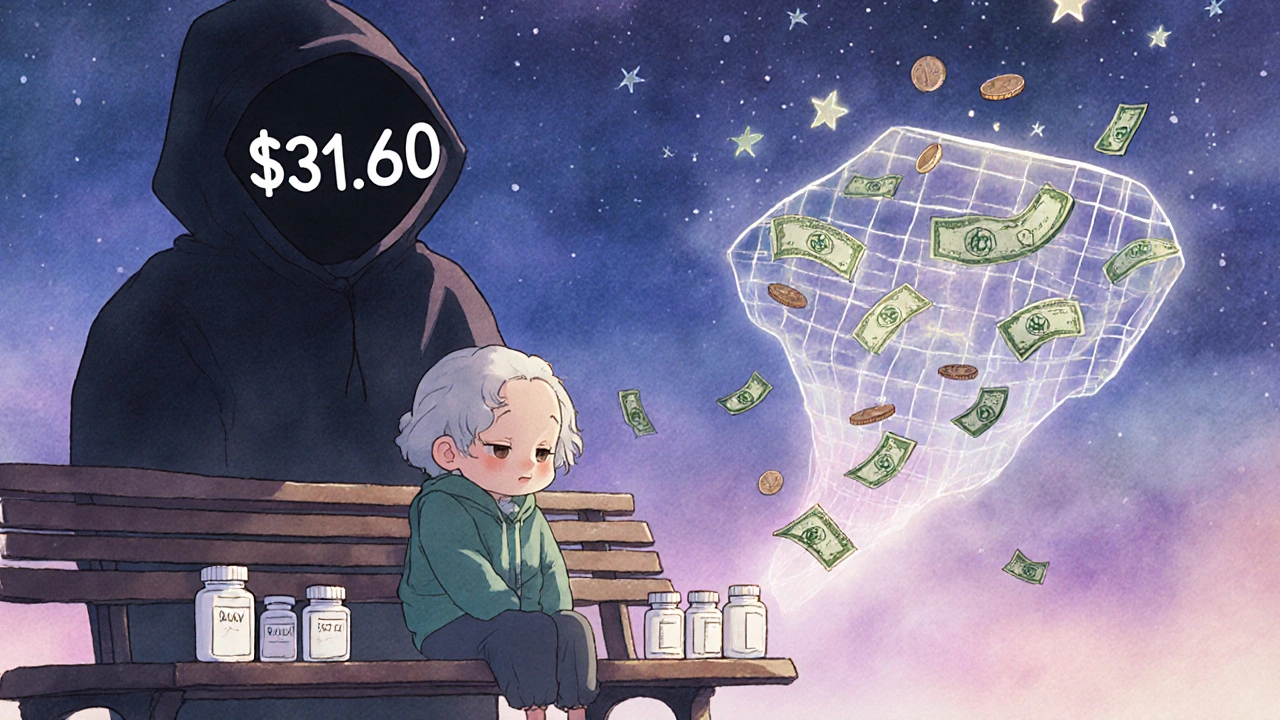
The PBS doesn’t give you free medicine. It caps what you pay. As of July 2024, general patients pay $31.60 per script, while concession card holders pay just $7.70. These amounts are adjusted yearly based on inflation, but in 2025, the government froze the general co-payment to save patients money. Starting January 1, 2026, it drops again-to $25. That’s a $6.60 cut for every prescription, which adds up fast if you’re taking five medications a month.
There’s also a safety net. Once you’ve spent $1,571.70 out-of-pocket on PBS medicines in a calendar year, your co-payment drops to the concession rate-$7.70-even if you’re not eligible for a concession card. For people with chronic conditions like diabetes or high blood pressure, this can mean the difference between staying on treatment or skipping doses.
But here’s the catch: not all medicines are treated the same. About 42% of PBS-listed drugs are restricted to specific conditions, and 28% require prior approval from Medicare. That means your doctor has to fill out extra paperwork before the pharmacy can dispense the drug. For prescribers, this adds hours to their workweek. For patients, it can mean delays-sometimes weeks-before they get their medicine.
The Generic Market: 84% by Volume, But Only 22% by Value
Australia has one of the highest rates of generic medicine use in the world. By volume, 84% of off-patent prescriptions are filled with generics. That’s higher than the OECD average of 78%. But here’s where it gets surprising: generics make up only 22% of total PBS spending. Why? Because originator brands still cost far more, even after patents expire.
The PBS uses a clever trick to drive down prices: reference pricing. If five drugs treat the same condition, the government sets the subsidy based on the cheapest one. If you choose a more expensive brand, you pay the difference. This pushes pharmacists and doctors toward generics-and patients often follow.
After a drug loses patent protection, the price of generics plummets. Within a year of multiple generic entries, prices drop by an average of 62%. In cardiovascular drugs, the drop can hit 74%. Statins, for example, see near-total generic adoption within 18 months. But not all drug classes follow the same pattern. Biologics-complex, injectable drugs used for conditions like rheumatoid arthritis or cancer-still have low generic uptake, around 63%, because substitution rules are stricter and manufacturing is harder.
The top five generic manufacturers-Symbion, Sigma, Mylan, Aspen, and Hospira-control nearly 70% of the market. They’re not just competing on price. They’re racing to be the first to enter after patent expiry, because the first generic gets the biggest share of sales.

Why New Drugs Take So Long to Reach Patients
One of the biggest criticisms of the PBS is how slow it is. The average time from when a drug is approved globally to when it’s listed on the PBS is 587 days. That’s almost two years. In Germany, it’s 320 days. In Canada, 410.
Why the delay? The Pharmaceutical Benefits Advisory Committee (PBAC) reviews every drug for clinical effectiveness and cost-effectiveness. They use a benchmark of around AU$50,000 per quality-adjusted life year (QALY). That means: if a drug costs $150,000 and extends life by three years with good quality, it’s considered cost-effective. But if it costs $200,000 for the same benefit, it’s unlikely to get listed-unless it’s for a rare disease.
That’s where the Highly Specialised Drugs Program (HSDP) comes in. It’s a special pathway for ultra-rare conditions. But even here, there are eight strict criteria. Many drugs that pass the Therapeutic Goods Administration (TGA) approval still get stuck in the PBS ‘black hole’-waiting an average of 14.2 months to be listed. During that time, patients pay full price-often $1,850 or more out of pocket.
Who’s Left Behind? The Hidden Cost of Co-Payments
The PBS works well for most people. But for those who don’t qualify for concessions and don’t hit the safety net, it’s a financial burden.
In 2024, 12.3% of general patients-about 1.8 million Australians-said they skipped doses or didn’t fill prescriptions because of cost. That’s not just a statistic. It’s a retiree choosing between insulin and groceries. It’s a single parent cutting their child’s asthma inhaler use to save money. The Australian Council of Social Service found that 28% of low-income households with multiple chronic conditions reduced food spending to afford medicine.
Reddit threads from r/AusFinance are full of stories like this: one user, a self-funded retiree, pays $158 a month just in co-payments for five medications. That’s over $1,900 a year. No safety net yet. No concession. Just a $31.60 bill every time they walk into the pharmacy.
On the flip side, nurses and pharmacists report that the safety net has been a game-changer for their patients. Once someone hits that threshold, their co-payment drops to $7.70. For many, that’s the moment they stop choosing between meds and meals.
What’s Changing in 2025 and Beyond
The PBS is evolving. In November 2025, the HSDP will relax two of its eight criteria for rare disease drugs, making it easier for patients with ultra-rare conditions to access treatment. The government also added 15 new drugs to the PBS in 2025, including Talazoparib for prostate cancer and Relugolix for endometriosis-expanding access to 150,000 more people.
The $1.2 billion allocated for new listings shows the government is trying to keep up with innovation. But spending is rising fast. PBS costs hit $13.5 billion in 2022-23 and are projected to reach $18.7 billion by 2029-30. The biggest drivers? High-cost biologics, expanded uses for existing drugs, and an aging population.
There’s also a push for digital reform. Services Australia now processes over 2 million authority requests a month online. But paper applications still take over a week to approve. The Department of Health is testing AI tools to flag inappropriate prescribing-$1.2 billion a year is spent on drugs that may not be needed, according to the Auditor-General.
The Bigger Picture: Is the PBS Sustainable?
Experts agree: the PBS is one of the most efficient pharmaceutical systems in the world. It saves Australians an estimated $13 billion a year in out-of-pocket costs. Without it, drug prices would be closer to U.S. levels-where a single insulin pen can cost $300.
But the system is under pressure. The cost-per-QALY threshold is flexible, but not infinite. As new cancer drugs cost $100,000 or more per year, the PBAC faces impossible choices. Should it fund a drug that gives a few extra months of life-or invest that money in five cheaper drugs that help hundreds?
And while generics keep prices low, the system still relies on originator companies to innovate. If the PBS becomes too restrictive, pharmaceutical firms may skip Australia altogether. That’s already happening with some rare disease drugs.
The challenge isn’t just about money. It’s about fairness. Can Australia keep its promise of universal access when the cost of medicine keeps climbing? The answer will shape healthcare for a generation.
What is the PBS in Australia?
The Pharmaceutical Benefits Scheme (PBS) is Australia’s government program that subsidizes the cost of prescription medicines for eligible residents. It ensures that essential drugs are affordable by covering most of the cost, with patients paying a co-payment. Over 5,400 medicines are listed, and nearly 87% of all prescriptions are subsidized through the PBS.
How much do Australians pay for PBS medicines in 2025?
As of July 2024, general patients pay $31.60 per prescription, and concession card holders pay $7.70. These amounts are indexed to inflation but were frozen in 2025. Starting January 1, 2026, the general co-payment will drop to $25.00 under the National Health Amendment (Cheaper Medicines) Bill 2025.
What is reference pricing in the PBS?
Reference pricing groups similar medicines together and sets the government subsidy based on the cheapest option. If you choose a more expensive brand, you pay the difference. This encourages the use of generics and keeps overall costs down. It’s a key reason Australia has one of the highest generic medicine use rates in the world.
Why are some medicines not available on the PBS right away?
New drugs must go through review by the Pharmaceutical Benefits Advisory Committee (PBAC), which assesses clinical effectiveness and cost-effectiveness. The average time from global approval to PBS listing is 587 days. Some drugs get stuck in a bureaucratic delay called the ‘PBS black hole,’ where they’re approved by the TGA but not yet listed, forcing patients to pay full price for over a year.
Are generic drugs as effective as brand-name drugs in Australia?
Yes. Generic drugs in Australia must meet strict standards set by the Therapeutic Goods Administration (TGA) to prove they are bioequivalent to the original brand. They contain the same active ingredient, in the same dose, and work the same way. The difference is usually only in price, packaging, or inactive ingredients. Most Australians safely use generics every day.
How does the PBS safety net work?
Once you’ve spent $1,571.70 on PBS medicines in a calendar year, your co-payment drops to the concession rate ($7.70) for the rest of the year-even if you’re not eligible for a concession card. This protects people with chronic illnesses from high out-of-pocket costs. The safety net resets each January 1.
Can international visitors use the PBS?
Yes, visitors from 11 countries with reciprocal health agreements can access PBS-subsidized medicines. These include New Zealand, the UK, Ireland, Sweden, the Netherlands, Finland, Italy, Malta, Norway, Slovenia, and Belgium. They must present a valid passport and proof of eligibility from their home country’s health system.
What is the difference between PBS and private health insurance?
The PBS covers the cost of listed prescription medicines, regardless of whether you have private health insurance. Private health insurance doesn’t cover PBS medicines-it only helps with hospital stays, dental, and extras. You can have private insurance and still rely on the PBS for your prescriptions. In fact, most Australians use both.







mike tallent
November 18, 2025 AT 08:12Just want to say the PBS is one of those things Americans don’t get until they’ve been through a medical crisis. I had a friend in Sydney who was on 6 meds for diabetes and heart stuff - paid $7.70 a script. Here? Same meds, $400 a month. No joke. 🇦🇺 got it right.
Joyce Genon
November 18, 2025 AT 22:37Oh please. The PBS isn’t ‘efficient’ - it’s just a slow, bureaucratic mess that delays life-saving drugs for years while people die waiting. And don’t even get me started on how they ‘reference price’ biologics - it’s not innovation, it’s price suppression disguised as fiscal responsibility. The government’s just playing games with people’s lives.
John Wayne
November 20, 2025 AT 19:35Reference pricing sounds clever until you realize it’s just a way to force patients into inferior generics that may not have the same bioavailability. And the 587-day approval window? That’s not due diligence - that’s institutional inertia. If this were a tech product, it’d be laughed out of the market.
Julie Roe
November 21, 2025 AT 03:44I work in pharmacy and I’ve seen the safety net save lives. I had a 72-year-old woman come in last month - she’d been skipping her blood pressure med because she couldn’t afford it. Hit the safety net in March, now she’s got her pills every 28 days like clockwork. She cried when I told her her co-pay dropped to $7.70. That’s not policy. That’s humanity.
And yeah, generics? They’re fine. TGA doesn’t mess around. I’ve compared blood levels in patients switching from brand to generic - identical. The only difference? Their wallet doesn’t cry.
Don’t let the naysayers scare you. The system’s not perfect, but it’s working for millions. And that $25 co-pay in 2026? Long overdue. We need more of that, not less.
jalyssa chea
November 22, 2025 AT 22:51Gary Lam
November 24, 2025 AT 06:34So Australia’s got a socialist drug program and y’all still think the US system is ‘free market’? 😂
Look, I get it - Americans think ‘government intervention’ = tyranny. But when your insulin costs more than your rent, maybe it’s time to admit that capitalism doesn’t work for life-saving stuff. The PBS is basically the anti-USA. And honestly? I’m jealous.
Peter Stephen .O
November 25, 2025 AT 04:11Let’s talk about the real magic trick here - generics at 84% volume but only 22% of cost. That’s not luck, that’s strategy. The PBS is basically playing 4D chess with Big Pharma. Let ‘em patent, then drop the hammer with reference pricing. First generic in? They get the gold mine. Everyone else? Fight over crumbs.
And biologics? Yeah, they’re the elephant in the room. You can’t just slap a generic on a protein that’s harder to replicate than a SpaceX rocket. But the HSDP tweak in 2025? That’s the quiet revolution. They’re finally realizing: if you want innovation, you gotta pay for it - even if it’s $200k a year.
Also - AI flagging inappropriate scripts? 1.2 billion wasted? That’s the real scandal. Not the co-pay. The waste. Fix that first.
Andrew Cairney
November 26, 2025 AT 23:37EVERYTHING ABOUT THE PBS IS A LIE. The ‘low co-pay’? It’s a trap. They let you think you’re safe until you hit the safety net - but guess what? They track EVERY SINGLE PRESCRIPTION. Your data’s in a federal database. They know when you’re on 5 meds. They know your income. They know if you’re a ‘high utilizer.’ And when you hit that $1571 threshold? That’s when they flag you for ‘risk profiling.’
And don’t tell me generics are safe. They’re made in India and China. Same active ingredient? Maybe. But the fillers? The binders? The heavy metals? No one’s testing that. This is chemical warfare on the poor. I’ve seen the leaks. They’re replacing lactose with cheap starch that causes inflammation. You think you’re saving money? You’re poisoning yourself.
And the 587-day delay? That’s not bureaucracy. That’s deliberate. They’re waiting for you to die so they don’t have to pay.
Rob Goldstein
November 28, 2025 AT 09:35From a clinical pharmacology standpoint, the PBS reference pricing model is one of the most elegant cost-containment mechanisms in global health. The key is the bioequivalence threshold - 80-125% AUC and Cmax range - which the TGA enforces with brutal precision. That’s why generics work. Not because they’re cheap, but because they’re scientifically identical.
The real bottleneck? PBAC’s QALY threshold. $50k/QALY is conservative, yes, but it’s not arbitrary. It’s anchored to Australia’s GDP per capita and willingness-to-pay studies. The problem isn’t the model - it’s the rising cost of novel therapies. CAR-T, gene therapies - those are the future fiscal stressors. The PBS is doing its job. The system needs recalibration, not dismantling.
vinod mali
November 29, 2025 AT 13:25in india we dont have anything like this. my dad pays $200 for his heart med. i wish we had a pbs. i just read this and felt lucky for australian people. even if it's not perfect, its way better than nothing.
Jennie Zhu
December 1, 2025 AT 02:52While the Pharmaceutical Benefits Scheme demonstrates commendable structural efficiency in terms of population-level cost containment and equitable access, the fiscal sustainability of the current QALY-based evaluation framework is increasingly untenable in the context of high-cost, low-prevalence therapeutics. The marginal cost-effectiveness ratio is approaching an inflection point wherein the opportunity cost of funding one novel biologic may preclude the provision of multiple lower-cost, high-impact interventions for prevalent chronic conditions. A dynamic, tiered pricing model calibrated to disease burden and socioeconomic impact may offer a more nuanced solution.
Kathy Grant
December 1, 2025 AT 22:10I used to think the PBS was just about money. Then my sister got diagnosed with MS. She was on a drug that cost $1,800 a month. We didn’t qualify for concessions. We didn’t hit the safety net. For 14 months, we paid. Every single month. We sold her car. We moved in with my mom. We skipped vacations. We ate rice and beans.
When the drug finally got listed? She cried. Not because she got it cheap. Because she didn’t have to choose anymore.
That’s not policy. That’s grace.
And yeah, the delays? The bureaucracy? The corporate lobbying? It’s all ugly. But for people like her - the ones who don’t have a voice in the debate - the PBS is the only thing standing between them and ruin.
Don’t fix it to be perfect. Fix it to be faster. And kinder.
Robert Merril
December 3, 2025 AT 00:53mike tallent
December 4, 2025 AT 00:49Love that you mentioned the safety net. My aunt hit it last year after her chemo meds. Went from $31.60 to $7.70. She said it felt like someone gave her back her dignity. That’s what this system does - it doesn’t just pay for meds. It pays for peace of mind.