Every year, generic drugs make up 84% of all prescriptions filled in the U.S. Yet, if you walk into a pharmacy and ask someone what they think of these medications, you’ll likely hear hesitation. "Are they safe?" "Do they really work the same?" "What if something went wrong?" These aren’t just random fears. They’re shaped by what people read, see, and hear in the news.
Why the News Keeps Scaring People
Headlines like "Contaminated Generic Drugs Reveal an Urgent Public Health Crisis" or "How Some Generic Drugs Could Do More Harm Than Good" don’t just grab attention-they stick in your mind. A 2019 Commetric analysis found that media stories about generic drugs are far more likely to focus on rare safety scares than on the overwhelming evidence that they work just as well as brand-name versions. And when they do mention safety, they rarely explain that the FDA holds generics to the same strict standards as the originals. Here’s the twist: most of these stories use the brand name. You’ll read about "Lipitor" instead of "atorvastatin," even though the generic version is the exact same active ingredient. This isn’t just sloppy reporting-it’s misleading. When patients hear about "Lipitor" causing side effects, they assume the generic version is different. It’s not. But the language tricks the brain into thinking it is. A 2014 JAMA Network study found that only 2% of U.S. newspapers had a written policy requiring reporters to use generic names. Even worse, nearly all of them used brand names by default. That means readers are being trained to associate quality and safety with brand names, not science.The Real Gap: Knowledge, Not Science
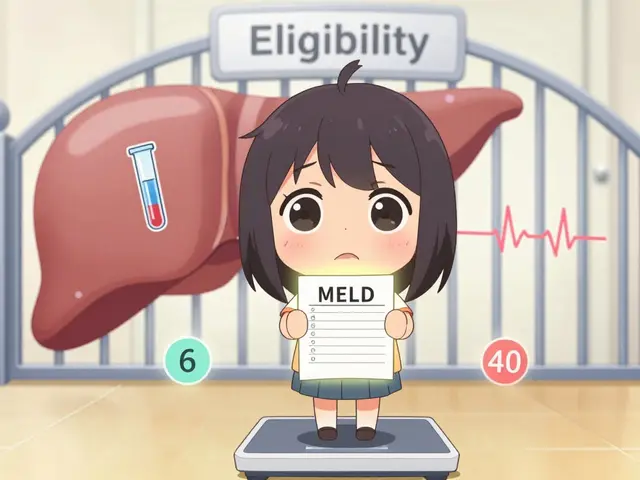
The science is clear. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also prove they’re absorbed into the body at the same rate and to the same extent. That’s not a guess. It’s a legal requirement backed by testing. But public understanding? That’s where things fall apart. A 2023 study published in PMC found that only 17% of people could correctly identify a generic medicine by its packaging. About 40% couldn’t tell the difference between a generic and a brand-name pill, even when shown side-by-side. And this isn’t because people are dumb-it’s because no one ever taught them. Most people don’t know that the FDA inspects generic manufacturing plants just as often as brand-name ones. They don’t know that many brand-name drugs are actually made in the same factories as generics. They don’t know that the FDA has approved over 20,000 generic drugs since 1984-and not one has been pulled for being less effective than its brand counterpart.When Bad News Hits, People Switch Back to Brand
Here’s something counterintuitive: patients who get bad health news-like a cancer diagnosis or a heart condition-are more likely to reject generics, even if they cost half as much. A 2023 University of Texas at Dallas study tracked patients after receiving serious health test results. In the first 90 days, they were 32% more likely to request the brand-name drug-even when their insurance didn’t cover it. Why? Because when you’re scared, you don’t want to take a chance. You want the name you recognize. And the media has spent decades making "brand" feel safer. This isn’t just about money. It’s about control. When you’re facing a life-changing diagnosis, choosing the brand-name drug feels like taking charge. Choosing the generic feels like settling. But the truth? You’re not settling. You’re getting the exact same medicine.
Doctors and Pharmacists Are the Missing Link
The one thing that actually changes people’s minds? Talking to their doctor or pharmacist. A 2015 systematic review found that patient trust in their healthcare provider almost always overrides their fear of generics. If your doctor says, "This generic is identical to the brand," and explains why, patients accept it. But if they just hand you the pill without saying anything? Doubt creeps in. Pharmacists are especially powerful here. They’re the last person you talk to before taking the medicine. And they know more about drug formulations than almost anyone. A 2023 US Pharmacist article showed that patients who had a 3-minute conversation with their pharmacist about generics were 50% more likely to stick with them long-term. Dr. Sarah Ibrahim from the FDA says it plainly: "Many of these beliefs come from uncertainty about how the generic differs from the brand-name drug." The fix? Simple: tell people there’s no meaningful difference. Not "it’s probably the same." Not "it’s close enough." Say it’s the same. Because it is.What the Media Gets Right (and What It Doesn’t)
Let’s be fair: media coverage isn’t all bad. When outlets report on price gouging-like when a generic drug jumps from $10 to $500 overnight-that’s important. The public needs to know when companies abuse the system. But those stories rarely mention the bigger picture: that when three or more companies make the same generic drug, prices drop by an average of 20%, according to a 2023 HHS ASPE report. The problem isn’t that the media covers drug prices. It’s that they rarely explain how competition works. They show a spike, but not the fall that follows. They show one bad batch, but not the 99.9% that pass inspection. They show fear, but not facts. And here’s the quiet truth: most journalists aren’t trained in pharmacology. They don’t know what "bioequivalence" means. They don’t know that the FDA requires generics to be within 80-125% of the brand’s absorption rate. That’s not a loophole-it’s a tight, scientifically proven range. But without context, it sounds like a gamble.
How to Fight the Misinformation
You can’t control the headlines. But you can control what you believe-and what you tell others.- Ask your pharmacist: "Is this generic the same as the brand?" They’ll show you the FDA’s approval data. It’s not a sales pitch-it’s a legal requirement.
- Check the label: Generic pills often have different colors or shapes, but the active ingredient is always listed. Look for the name on the box-like "metformin," not "Glucophage."
- Don’t assume cost = quality: A $5 generic isn’t "cheap medicine." It’s medicine that’s been made efficiently, not marketed aggressively.
- Share the facts: If someone says, "I won’t take generics," ask them why. Then ask if they know the FDA requires them to be identical. Most people don’t.
It’s Not About Trust in Drugs. It’s About Trust in Information.
The real issue isn’t that people distrust generic drugs. It’s that they’ve been fed a steady diet of half-truths, sensational headlines, and silent omissions. They’ve been taught to equate familiarity with safety, and cost with compromise. But science doesn’t care about brand names. It only cares about what’s in the pill-and what it does in your body. The next time you see a headline screaming about a "dangerous generic," pause. Ask: Did they say what the drug actually is? Did they mention the FDA? Did they explain how many other companies make it? Did they say how much cheaper it is? If the answer is no, then you’re not reading a news story. You’re reading a fear tactic. And you deserve better than that.Are generic drugs really the same as brand-name drugs?
Yes. The FDA requires generic drugs to have the exact same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re absorbed into the body at the same rate and to the same extent. The only differences are in inactive ingredients like color or shape-none of which affect how the drug works.
Why do some people say generic drugs don’t work as well?
This belief often comes from media stories that focus on rare cases of contamination or price spikes, without explaining how common and safe generics are. Some people also confuse packaging differences or minor side effects with effectiveness. But large-scale studies show patients on generics are just as likely to get better-and more likely to stick with their treatment because it’s affordable.
Can I trust generics made overseas?
Yes. The FDA inspects all manufacturing facilities-whether they’re in the U.S., India, or China-before approving a generic drug. Over 80% of generic drugs sold in the U.S. are made overseas, and they’re held to the same standards as brand-name drugs made domestically. The FDA has no preference for where a drug is made, only that it meets safety and quality rules.
Why do pharmacists sometimes switch my brand to generic without asking?
In most cases, state laws allow pharmacists to substitute a generic for a brand-name drug unless the doctor specifically says "do not substitute." This is legal, safe, and saves money. Pharmacists are trained to know when substitution is appropriate. If you’re uncomfortable, ask them to explain why the switch was made-they’re required to help you understand.
Does insurance cover generics better than brand-name drugs?
Yes. Most insurance plans have lower co-pays for generics because they’re cheaper. Some even require you to try the generic first before approving the brand. This isn’t a trick-it’s a way to reduce overall healthcare costs so more people can afford treatment.
What should I do if I think my generic drug isn’t working?
Don’t assume it’s the drug. Talk to your doctor or pharmacist first. Sometimes, changes in how you feel are due to other factors-like stress, diet, or other medications. If you’re concerned, ask them to check if your prescription was filled correctly. Rarely, a person might react differently to inactive ingredients, but that’s uncommon and fixable with a different generic version.






Jessica Ainscough
December 3, 2025 AT 09:11Been taking generics for years. Never had an issue. My blood pressure med? Same as the brand. My cholesterol? Same. I don't get the fear. It's not magic, it's chemistry.
Josh Bilskemper
December 4, 2025 AT 11:25Media doesn't care about facts they care about clicks. Generic drugs are a boring story unless you can scream 'DANGER' in all caps. The FDA isn't perfect but it's not the enemy either. Stop letting headlines think for you.
dan koz
December 5, 2025 AT 06:04Back home in Nigeria we don't even have brand names most times. Just the generic. And we still live. Maybe the fear is a rich country luxury.
Katey Korzenietz
December 6, 2025 AT 08:14Someone needs to sue the media for psychological harm. This isn't journalism its fear porn. And people are paying with their health because they're too scared to save money.
Storz Vonderheide
December 8, 2025 AT 05:04My mom used to refuse generics until her pharmacist sat her down and showed her the FDA paperwork side by side. She cried. Not from sadness. From relief. Turns out she'd been overpaying for 12 years thinking she was getting something better. She now tells everyone.
Kevin Estrada
December 8, 2025 AT 20:08Wait wait wait. So you're telling me Big Pharma is secretly controlling the media to make us buy expensive pills? And the FDA is in on it? But then why do they let generics exist at all? This feels like a plot twist from a Netflix docu-series.
Michael Bene
December 9, 2025 AT 07:02Let me tell you about my cousin's aunt's neighbor who took a generic for anxiety and started seeing ghosts. No joke. She swore the pills were 'different.' Turned out she switched brands twice and the color changed. That's not the drug. That's her brain. And now she won't touch anything that isn't in a blue bottle.
Chris Jahmil Ignacio
December 11, 2025 AT 01:24It's not about science it's about control. The system wants you dependent on expensive branded drugs because that's where the profit is. The media is just the echo chamber. The FDA? A puppet. The real question is why do you trust a government agency that lets pharmaceutical companies lobby for tax breaks while you pay $500 for insulin
Casey Lyn Keller
December 12, 2025 AT 13:45I don't care what the FDA says. I've seen too many news stories about tainted generics. I'm not risking my life for $10 savings. If I can afford the brand I'm taking the brand. End of story.
Paul Corcoran
December 14, 2025 AT 09:47My daughter's pediatrician explained generics to her like this: 'It's like buying the same exact cake but without the fancy wrapping and the logo on top. The sugar and flour are the same. The taste is the same. You're just not paying for the sticker.' She got it immediately. Maybe we need more doctors who talk like humans.
Ethan McIvor
December 15, 2025 AT 13:04It's funny how we trust the same science that put a man on the moon but doubt the same science that says a pill is safe. We want to believe in miracles but not in math. Maybe the real problem isn't the drugs. It's our relationship with knowledge itself.
Jessica Ainscough
December 16, 2025 AT 21:02Just had my pharmacist explain this to me again. Said the same factory makes both. The brand gets the fancy box. The generic gets the plain one. Same pills. Same quality. I just saved $42 this month. I'm not mad. I'm grateful.