When your brand-name medication switches to a generic version, it’s not just a label change-it’s a moment that can affect how you feel, how much you pay, and whether your treatment stays effective. You might not even notice the switch unless your pill looks different, costs less, or suddenly stops working the way it used to. That’s why communicating with your pharmacy during a generic transition isn’t optional-it’s essential.
Why Generic Switches Happen
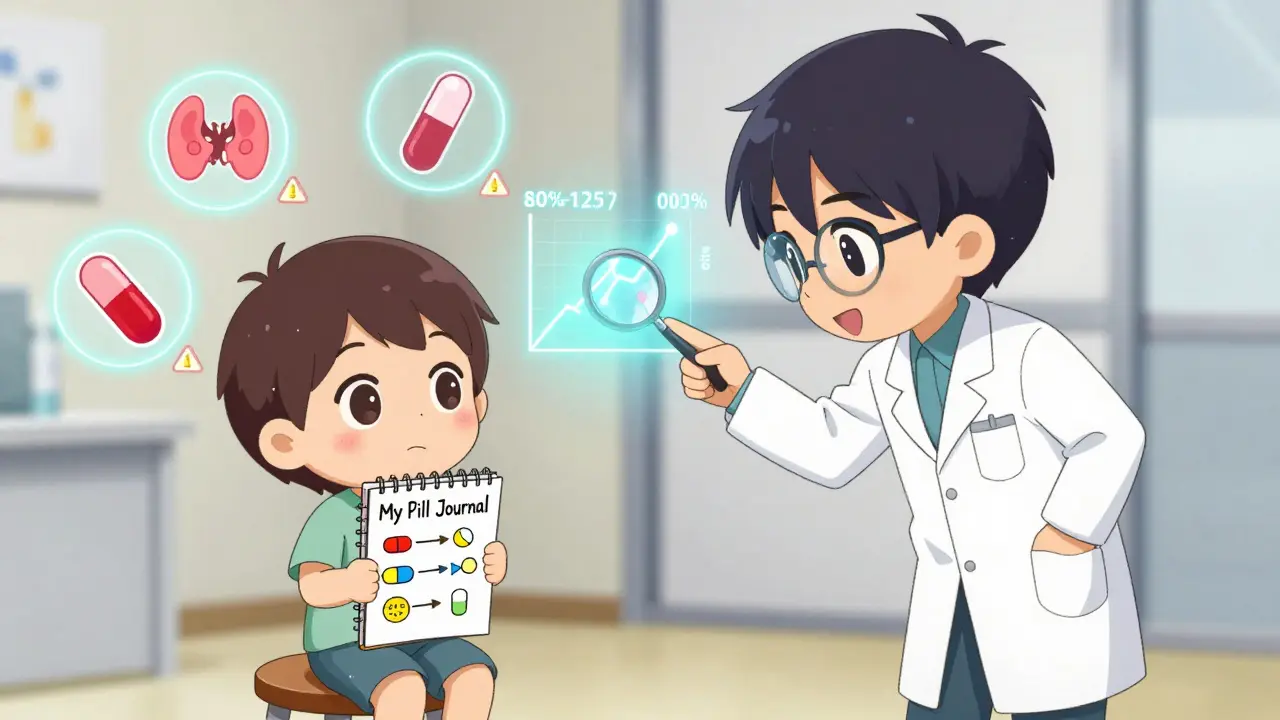
Generic drugs aren’t cheaper because they’re lower quality. They’re cheaper because they don’t need to repeat the decade-long, billion-dollar clinical trials that brand-name drugs do. Once a patent expires, other companies can make the same active ingredient under the FDA’s strict rules. The FDA requires generics to deliver the same amount of medicine into your bloodstream at the same speed as the brand. That’s called bioequivalence. The acceptable range? Between 80% and 125% of the brand’s performance. That’s tight. But even within that range, small differences can matter-especially for drugs where the margin between effective and dangerous is thin.What Changes When You Switch
The active ingredient stays the same. But everything else might not. The color, shape, size, or markings on the pill can change. The inactive ingredients-like fillers, dyes, or preservatives-can be different. For most people, this makes no difference. But for some, those tiny changes can cause side effects or make the drug work differently. That’s why people on medications like levothyroxine (for thyroid), warfarin (a blood thinner), or antiepileptics like levetiracetam (Keppra) need to pay extra attention. A 2021 study in JAMA Internal Medicine found that nearly 1 in 10 patients who switched from brand to generic antiepileptic drugs had a seizure they didn’t have before. That’s not common, but it’s real. And it’s why your pharmacist needs to know your history.What Your Pharmacist Does (and Doesn’t Do)
Your pharmacist doesn’t just fill the prescription. They’re the last line of defense before you take the pill. When a generic becomes available, the pharmacy’s system automatically switches your prescription unless your doctor says otherwise. But here’s the catch: if your insurance plan has a tiered formulary, the generic might be the only option covered unless you pay more. That’s why your pharmacist checks your coverage before dispensing. They also check for drug interactions. They verify your dosage. They look at your full medication list. And if you’ve had problems with generics before, they need to know. That’s why you should always bring your updated medication list to every visit-even if you think you’ve told them before.When to Start Talking to Your Pharmacy
Don’t wait until your last bottle is empty. Start the conversation at least 30 days before your brand-name drug runs out. That gives your pharmacy time to:- Check if your insurance will cover the generic (or if you need prior authorization to stay on brand)
- Confirm whether your doctor has placed a "Do Not Substitute" note on your prescription
- See if there’s a patient assistance program from the generic manufacturer
- Coordinate with your specialty pharmacy if you’re on a complex medication
What to Ask Your Pharmacist
When your pharmacist tells you your medication is switching, don’t just say "okay." Ask these five questions:- Is this a generic version of my current drug? If so, what’s the brand name?
- Will this change how I take it-dose, timing, or instructions?
- Could the inactive ingredients affect me? I’ve had reactions to dyes or fillers before.
- Is there a difference in cost? Can I get it cheaper through a mail-order or discount program?
- What should I watch for? What side effects might be new?
What to Do If Something Feels Off
If you notice new side effects, reduced effectiveness, or strange symptoms after switching, don’t assume it’s "just in your head." Track it. Write down:- When you started the new pill
- What changed-sleep, mood, energy, seizures, blood pressure, etc.
- Any differences in pill appearance
How to Avoid Confusion and Mistakes
Pills look different. That’s normal. But it’s also confusing. A 2022 survey found that 37% of patients hesitated to take a new pill just because it looked different. That’s dangerous. To avoid this:- Always check the pill imprint code (letters/numbers on the pill) against the label
- Ask your pharmacist to show you the new pill before you leave
- Use a pill organizer labeled with the drug name, not just the day
- Take a photo of your old pill and the new one on your phone for comparison

Insurance and Costs: What You Need to Know
Generics save money-big time. Medicare beneficiaries save an average of $265 per medication annually when switching. Commercial insurers save even more. But that doesn’t mean you’ll always get the cheapest option. Many plans require prior authorization to keep you on brand-name drugs. If your doctor doesn’t submit that paperwork, the pharmacy will automatically switch you. That’s why you need to confirm your plan’s rules before the transition. Some generic manufacturers offer discount cards or co-pay assistance programs. Ask your pharmacist if one exists for your new medication. You might get it for $5 or even free.What’s Changing in 2026
The DEA changed the rules in 2023: you can now request an electronic transfer of your controlled substance prescription (like opioids or ADHD meds) between pharmacies without going back to your doctor. That’s huge. It means if your brand-name drug is discontinued and you need to switch pharmacies, you can move your prescription faster. EHR systems like Epic now flag potential generic switch issues automatically. Pharmacists get alerts if a patient has had problems before. And pilot programs at CVS and Walgreens are using blockchain to track generic transitions-helping patients see exactly which version they’re getting and when it changed. But tech doesn’t replace conversation. AI can flag risks, but only a pharmacist can hear your concern and say, "Let’s get you back on the brand. Your safety comes first."Bottom Line: Be Your Own Advocate
Generic drugs are safe, effective, and save billions. But they’re not identical in every way to the brand. Your body might react differently. Your insurance might not cover what you expect. Your pill might look unfamiliar. The best thing you can do? Talk to your pharmacist. Early. Often. Honestly. Don’t assume they know your history. Don’t assume the switch won’t affect you. Don’t wait until you feel worse to speak up. You’re not being difficult. You’re being smart. And in the world of medications, being smart can mean the difference between staying well-and having to go back to the doctor.Can I refuse a generic drug switch?
Yes. You can ask your pharmacist to fill your prescription with the brand-name drug instead. Your doctor may need to write "Do Not Substitute" on the prescription, or your insurance might require prior authorization. If the generic is the only covered option, you can pay out-of-pocket for the brand. Pharmacists are required to honor your request if you refuse the substitution.
Why does my generic pill look different?
Generic manufacturers must use different colors, shapes, or markings than the brand-name drug to avoid trademark violations. These changes don’t affect how the medicine works, but they can cause confusion. Always check the pill imprint code and confirm with your pharmacist that the new pill is the correct medication.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generics to meet the same strict standards for quality, strength, purity, and stability as brand-name drugs. Over 90% of prescriptions in the U.S. are filled with generics, and they’ve been used safely for decades. However, rare cases of different side effects or reduced effectiveness can occur due to variations in inactive ingredients or bioavailability-especially with narrow therapeutic index drugs.
What if I have an allergic reaction to a generic?
If you experience a new allergic reaction or side effect after switching, contact your pharmacist and doctor immediately. The issue may be caused by an inactive ingredient-like a dye, gluten, or lactose-that’s different in the generic. Your pharmacist can help identify which ingredient caused the reaction and find a generic version without it, or return you to the brand.
Can I switch back to the brand-name drug after trying the generic?
Yes. If the generic doesn’t work for you or causes side effects, you can ask your doctor to prescribe the brand-name drug again. Your pharmacist can help you file a formulary exception with your insurance, or you can pay out-of-pocket. Many patients successfully switch back-especially those on thyroid, seizure, or blood-thinning medications.
Does my pharmacy notify me before switching to a generic?
Not always. Many pharmacies automatically substitute generics unless the prescription says "Dispense as Written" or your insurance blocks it. That’s why it’s your job to ask. Call your pharmacy before your refill is due and say, "Is my medication switching to a generic?" Don’t wait for them to tell you.
Next Steps
- Call your pharmacy today and ask if any of your medications are switching to generics in the next 30 days.
- Write down the names, doses, and appearances of all your current pills.
- Ask your pharmacist for a printed list of your medications and their generic equivalents.
- If you’re on a high-risk drug (thyroid, seizure, blood thinner), schedule a follow-up with your doctor after switching.





Aysha Siera
January 18, 2026 AT 11:55The FDA doesn't control the fillers. Big Pharma owns the generic makers. You think this is coincidence?
rachel bellet
January 19, 2026 AT 05:07From a pharmacoeconomic standpoint, the bioequivalence threshold of 80–125% is statistically indefensible for narrow-therapeutic-index agents. The variance in Cmax and AUC introduces unacceptable interpatient variability, particularly in polypharmacy cohorts with altered hepatic metabolism. This isn't 'generic substitution'-it's clinical roulette.
Naomi Keyes
January 21, 2026 AT 01:47Have you considered that the color change alone-due to the use of FD&C dyes-can trigger psychological nocebo effects in patients with anxiety disorders? And yet, we don't test for that. We test for plasma concentrations, not perception. The pill looks different, so your brain says it's not working. That's not the drug's fault-it's the system's failure to account for cognitive bias.
Also, I've seen patients panic because the pill was oval instead of round. They stopped taking it. They ended up in the ER. The pill didn't change. Their fear did.
And don't get me started on how pharmacies don't document the manufacturer change in the EHR. If you switch from Mylan to Teva, that matters. But no one tracks it. It's all buried in a PDF invoice.
Why aren't we requiring barcode-scannable lot numbers on every prescription bottle? So you can trace the exact batch you took? Because we'd have to pay for it. And that's not profitable.
I once had a patient who had a seizure after switching from brand Keppra to a generic with magnesium stearate. She was lactose intolerant. The generic used lactose as a filler. The brand didn't. No one asked. No one checked. The pharmacist didn't know her history. That's not negligence. That's systemic abandonment.
And yet, we praise generics as 'cost-effective.' Cost-effective for whom? For insurers? For pharmacy benefit managers? Not for the person swallowing the pill.
There's a reason why Japan requires the same manufacturer for chronic meds. They get it. We don't.
And yes, I've filed 17 formulary exceptions. All approved. Because I refused to let bureaucracy decide my treatment.
You're not being difficult. You're being data-driven.
Ryan Otto
January 22, 2026 AT 08:08Let me be clear: the FDA’s bioequivalence standards are a charade. The 80–125% window is not a scientific boundary-it’s a political compromise. The same corporations that produce the brand-name drugs also produce the generics. The ‘independent’ labs? Owned by the same holding companies. The data? Selected. The trials? Underpowered. The real question isn’t whether generics work-it’s whether they were ever meant to work for you.
And don’t tell me about ‘inactive ingredients.’ That’s the most cynical euphemism in modern medicine. Fillers are not ‘inactive.’ They’re adjuvants. They’re carriers. They’re the silent variables your body never agreed to. Titanium dioxide? Propylene glycol? Corn starch? All of them can trigger immune dysregulation in susceptible individuals. But because they’re not ‘active,’ we ignore them.
And then there’s the supply chain. The active pharmaceutical ingredient (API) for most generics is manufactured in China or India. Do you know how many of those facilities have been cited for data falsification? Over 200 in the last decade. And yet, the FDA approves them anyway. Why? Because it’s cheaper. Because you’re too lazy to ask.
My cousin was on warfarin. Switched to generic. INR spiked to 7.2. Almost bled out. The pharmacist said, ‘It’s the same thing.’ It wasn’t. The crystal structure was different. The dissolution rate was off by 18%. The FDA doesn’t test that. They test plasma levels after a single dose in healthy volunteers. Not in a 72-year-old with renal impairment.
This isn’t about cost. It’s about control. The system wants you dependent on the pharmacy’s algorithm, not your own physiology. You think your doctor knows what’s in your pill? They don’t. The EHR doesn’t tell them. The label doesn’t tell them. Only you-and your pharmacist, if you’re lucky-know the truth.
And if you dare to complain? They’ll call you a ‘non-compliant patient.’
Wake up. The pill you’re swallowing isn’t medicine. It’s a corporate experiment.
Danny Gray
January 22, 2026 AT 18:38What if the real issue isn't the generic drug-but the fact that we've outsourced our bodily autonomy to a system that treats humans like data points? We don't ask if the pill feels right. We ask if it's covered. We don't track how we feel-we track refill dates. We've turned healing into a transaction, and now we're surprised when the body rebels?
Maybe the problem isn't the filler. Maybe it's that we stopped listening.
And if you think the pharmacist cares, you haven't worked a 12-hour shift with 200 scripts and 47 angry people yelling about their co-pays.
Who's really responsible here? The manufacturer? The insurer? Or the person who stopped asking questions because it was easier?
It's not about the pill. It's about the silence.
Wendy Claughton
January 23, 2026 AT 05:43I just want to say thank you for writing this. 💙 I switched from brand Keppra to generic last year and had three seizures in two weeks. I was terrified. I called my pharmacist and said, ‘This isn’t me.’ They listened. They called my neurologist. We switched back. My life is different now. I’m alive. Please, if you’re reading this and you feel ‘off’ after a switch-don’t second-guess yourself. Your body knows. Trust it. And don’t let anyone tell you it’s ‘all in your head.’ It’s not. You’re not crazy. You’re just paying attention.
Stacey Marsengill
January 23, 2026 AT 06:43Oh, sweet summer child. You think this is about pills? No. This is about the death of trust. The pharmaceutical industry doesn’t want you healthy. They want you dependent. Generics? A trap. A slow poison disguised as savings. You think your insurance cares? They care about quarterly profits. Your pharmacist? They’re paid per script. They don’t care if you live or die-just that you take the pill.
I’ve seen people die because they were switched to a generic with titanium dioxide. It’s not in the label. It’s not in the leaflet. But it’s in the pill. And your body? It remembers.
And now they’re putting blockchain on it? LOL. Like that fixes the fact that your life is being decided by a spreadsheet in a cubicle in New Jersey.
You’re not being ‘smart.’ You’re being the only one awake in a room full of sleepwalkers.
Tyler Myers
January 23, 2026 AT 20:30Generics are a scam. The FDA is owned by Big Pharma. The 'bioequivalence' study? 40 healthy college kids. Not your grandma with kidney disease. Not your kid with epilepsy. Just kids. Then they say 'it's the same.' It's not. It's never been the same. I've been on the same brand since 2010. I won't switch. I pay out of pocket. I'm not a lab rat. And neither are you.
Andrew McLarren
January 24, 2026 AT 11:48While the concerns raised regarding bioequivalence thresholds and inactive ingredient variability are empirically valid, it is imperative to acknowledge that the overwhelming majority of generic substitutions occur without adverse clinical consequences. The FDA’s regulatory framework, though imperfect, remains among the most rigorous globally. The anecdotal evidence of adverse outcomes, while deeply concerning, must be contextualized within population-level data demonstrating safety and efficacy across hundreds of millions of prescriptions annually. A balanced approach-combining patient advocacy with evidence-based practice-is not only prudent but ethically obligatory.
That said, the systemic failure to document manufacturer changes in electronic health records remains a critical gap requiring urgent policy intervention.
Pat Dean
January 25, 2026 AT 01:18Why are we even talking about this? America spends more on healthcare than any country on earth-and we’re still letting foreign factories make our pills? That’s not innovation. That’s surrender. If you want real medicine, buy American. Pay the extra $10. Support our workers. Don’t let China decide if your seizure meds work. This isn’t about cost. It’s about sovereignty. And if you’re okay with that, you’re not just naive-you’re complicit.