After giving birth, many women feel exhausted, overwhelmed, and emotionally drained. It’s normal. But what if your fatigue doesn’t go away? What if you’re losing weight but can’t eat enough, or gaining weight despite eating less? What if you’re cold all the time, your hair is falling out, or your heart races for no reason? These aren’t just signs of being a new mom-they could be symptoms of postpartum thyroiditis, a hidden thyroid condition that affects 5 to 10% of women after childbirth.
What Exactly Is Postpartum Thyroiditis?
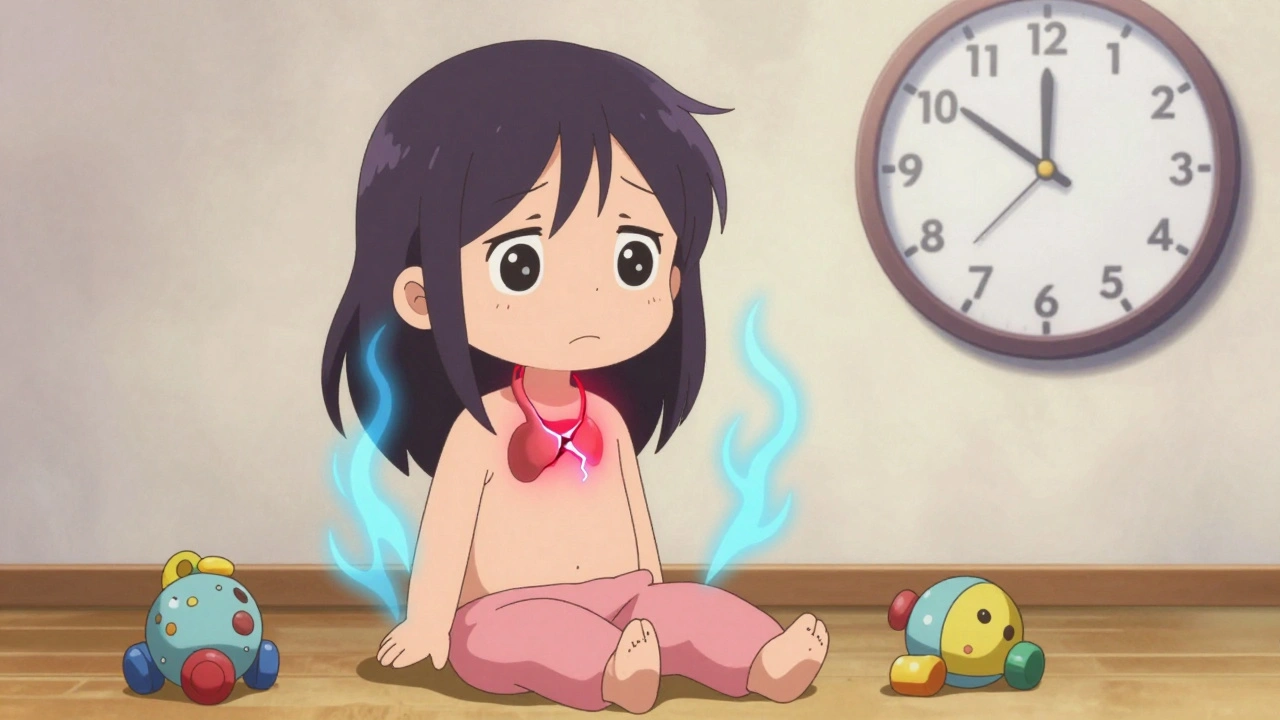
Postpartum thyroiditis is an autoimmune inflammation of the thyroid gland that happens within the first year after delivery, miscarriage, or abortion. It’s not caused by infection or poor diet-it’s your immune system mistakenly attacking your thyroid. This happens because pregnancy suppresses your immune system to protect the baby, and after birth, it rebounds aggressively. If you already have thyroid antibodies (especially TPO antibodies) before or during pregnancy, your risk jumps significantly.
Unlike Hashimoto’s or Graves’ disease, which are permanent, postpartum thyroiditis is usually temporary. About 70 to 80% of women return to normal thyroid function within 12 to 18 months. But for 20 to 30%, it leads to lifelong hypothyroidism. That’s why recognizing it early matters.
The Two-Phase Pattern: Hyperthyroidism, Then Hypothyroidism
This condition doesn’t hit you all at once. It comes in two phases-often with a quiet period in between.
Phase One: Hyperthyroidism (1 to 4 months postpartum)
Your thyroid gets damaged by immune cells, causing stored hormones to leak out. This gives you a temporary surge of thyroid hormone-like your thyroid is overworking. Symptoms include:
- Heart rate over 100 beats per minute
- Feeling hot when others are cold
- Unexplained weight loss (4-7 pounds)
- Tremors in your hands
- Insomnia or trouble sleeping
- Anxiety or nervousness
Here’s the catch: up to half of women don’t even notice these symptoms. Doctors often mistake them for stress, lack of sleep, or anxiety. But if you’re having a racing heart and can’t sleep despite a newborn sleeping through the night, it’s worth checking.
Phase Two: Hypothyroidism (4 to 8 months postpartum)
After the hormone stores are drained, your thyroid can’t keep up. Now you’re running low. This phase hits harder and lasts longer-often 9 to 12 months. Symptoms include:
- Extreme fatigue (89% of women report this)
- Feeling cold all the time
- Constipation
- Dry, flaky skin
- Hair thinning or shedding
- Weight gain (5-10 pounds) without change in diet
- Brain fog-trouble focusing, remembering names, or making simple decisions
This phase is where most women finally seek help. But even then, many are told they’re just tired from being a new mom. The problem? This fatigue doesn’t improve with rest. It doesn’t go away when the baby starts sleeping longer. It’s biological.
Who’s at Risk?
Not every woman gets postpartum thyroiditis. But certain factors make it much more likely:
- Having type 1 diabetes (risk jumps to 25-30%)
- Previous episode of postpartum thyroiditis (40% chance it comes back)
- High levels of TPO antibodies during pregnancy
- Family history of autoimmune thyroid disease
- Other autoimmune conditions like lupus or rheumatoid arthritis
If you fall into any of these categories, you should ask your doctor for a TPO antibody test during pregnancy or right after delivery. A simple blood test at 10 weeks postpartum can predict 70% of future cases.
How Is It Diagnosed?
There’s no single test that confirms it. Diagnosis relies on three things:
- Symptoms-matching the two-phase pattern
- Thyroid function tests-TSH and free T4 levels
- TPO antibody test-positive in 80-90% of cases
During the hyperthyroid phase, your TSH will be low (under 0.4 mIU/L) and free T4 high. In the hypothyroid phase, TSH rises above 4.5 mIU/L and free T4 drops. The TPO antibody test tells you it’s autoimmune-not just stress or exhaustion.
What it’s not: Graves’ disease. That’s another autoimmune thyroid condition, but it causes a goiter (swollen neck), bulging eyes, and high radioactive iodine uptake. Postpartum thyroiditis shows almost no iodine uptake-your thyroid is damaged, not overactive.

Why Misdiagnosis Is Common-and Dangerous
Doctors miss this condition all the time. A 2022 study found that 65% of primary care providers first blame symptoms on "new mom stress." On Reddit’s thyroid community, 78% of women said they were initially diagnosed with postpartum depression. One woman told me she saw three doctors before someone ordered a blood test.
Why does this matter?
- Antidepressants won’t fix your thyroid.
- Unmanaged hypothyroidism can affect your milk supply-38% of women report decreased production.
- It can worsen anxiety, brain fog, and depression-making it harder to bond with your baby.
- If left untreated, permanent hypothyroidism becomes more likely.
According to Cleveland Clinic data, 40% of women initially misdiagnosed with depression were prescribed antidepressants. Their symptoms didn’t improve. Once they got thyroid treatment, they felt like a new person.
Treatment: What Works and What Doesn’t
You don’t need surgery or radiation. Treatment is simple-but depends on the phase.
During hyperthyroidism: Most women don’t need medication. The phase is short, and your body will reset. If your heart is racing badly or you’re anxious, a low-dose beta-blocker (like propranolol) can help control symptoms for a few weeks. No antithyroid drugs like methimazole-those are for Graves’ disease and won’t help here.
During hypothyroidism: If your TSH is above 10 mIU/L, or you’re symptomatic with TSH over 4.5, you’ll likely need levothyroxine (synthetic thyroid hormone). Most women take it for 6 to 12 months. Then, your doctor will slowly stop it and retest. About 70-80% won’t need it again. But if your TPO antibodies are high and your thyroid doesn’t recover, you’ll need it for life.
Important: Don’t stop levothyroxine on your own. Even if you feel better, your thyroid might still be damaged. Stopping too soon can lead to a rebound in symptoms or permanent dysfunction.
Can You Breastfeed While on Treatment?
Yes. Levothyroxine is safe during breastfeeding. Only tiny amounts pass into breast milk-far less than what your baby naturally produces. Beta-blockers like propranolol are also considered safe in low doses. Always tell your doctor you’re breastfeeding so they choose the right medication and dose.

What Happens Long-Term?
Most women recover. But 20-30% develop permanent hypothyroidism. That means lifelong medication-but it’s manageable. Once you’re on the right dose of levothyroxine, your energy, mood, and weight stabilize. You can live normally.
Women who’ve had postpartum thyroiditis are at higher risk for future thyroid problems. One study showed that 20% develop thyroid issues again within 10 years-even without another pregnancy. That’s why annual TSH checks are recommended after recovery.
What Should You Do Now?
If you’re within a year of giving birth and feel off-really off-don’t wait. Ask for a thyroid panel: TSH, free T4, and TPO antibodies. Do it at 6 to 12 weeks postpartum. If you have diabetes or a history of thyroid issues, ask for it even earlier.
If your doctor says, "It’s just stress," ask: "Could this be thyroiditis?" Show them the symptoms list. Bring up the fact that 5-10% of women get this. Most doctors aren’t trained to think of it-but they’ll listen if you come prepared.
And if you’ve been told you have postpartum depression but antidepressants aren’t helping? Get your thyroid checked. You might be one blood test away from feeling like yourself again.
What’s Changing in 2025?
Experts are pushing for routine screening. UCLA’s Dr. Angela Leung predicts universal TSH testing at 6 and 12 weeks postpartum will become standard within the next five years. Why? Because catching it early saves money-$2,300 per case in avoided misdiagnosis and complications.
Some clinics now offer digital symptom trackers. You log your energy, sleep, weight, and mood daily. The system flags patterns that match thyroiditis. In pilot studies, it cut diagnosis time by 40%.
But access is still unequal. In low-income countries, 65% of women can’t get thyroid testing at all. That’s a global health gap that needs fixing.
For now, the best thing you can do is know your body. If something feels wrong after birth, don’t ignore it. Your thyroid doesn’t lie. And neither should your instincts.





Aileen Ferris
December 9, 2025 AT 20:19Nikki Smellie
December 10, 2025 AT 01:36David Palmer
December 11, 2025 AT 08:05Doris Lee
December 12, 2025 AT 16:00Michaux Hyatt
December 14, 2025 AT 03:19Raj Rsvpraj
December 14, 2025 AT 18:42Neelam Kumari
December 15, 2025 AT 22:41Stephanie Maillet
December 16, 2025 AT 08:39Michelle Edwards
December 17, 2025 AT 22:03Sarah Clifford
December 18, 2025 AT 11:30