Rivastigmine Dosing Calculator
Rivastigmine Titration Schedule
Start with 1.5 mg twice daily and gradually increase over 4-8 weeks to reach the target dose of 6 mg twice daily, as tolerated.
Initial dose for tolerance building
First titration step
Second titration step
Target maintenance dose
Side Effect Management
Common Side Effects
GI symptoms (nausea, vomiting, diarrhea) are most common, especially with oral formulation.
Management Tips
- Take with food to reduce nausea
- Consider transdermal patch to minimize GI side effects
- Slow titration helps improve tolerance
- Stay hydrated and maintain healthy diet
Expected Benefits
2-3 Point MMSE Improvement
Over 24 weeks (compared to placebo)
Key Benefits:
- Modest cognitive improvements
- Improved attention and executive function
- Slowed progression in early-moderate stages
- Reduced symptom burden for caregivers
Monitoring Your Progress
Regular cognitive assessments help track treatment response. Common tools include:
Check with your healthcare provider every 3-6 months to assess benefit and side effects.
Quick Takeaways
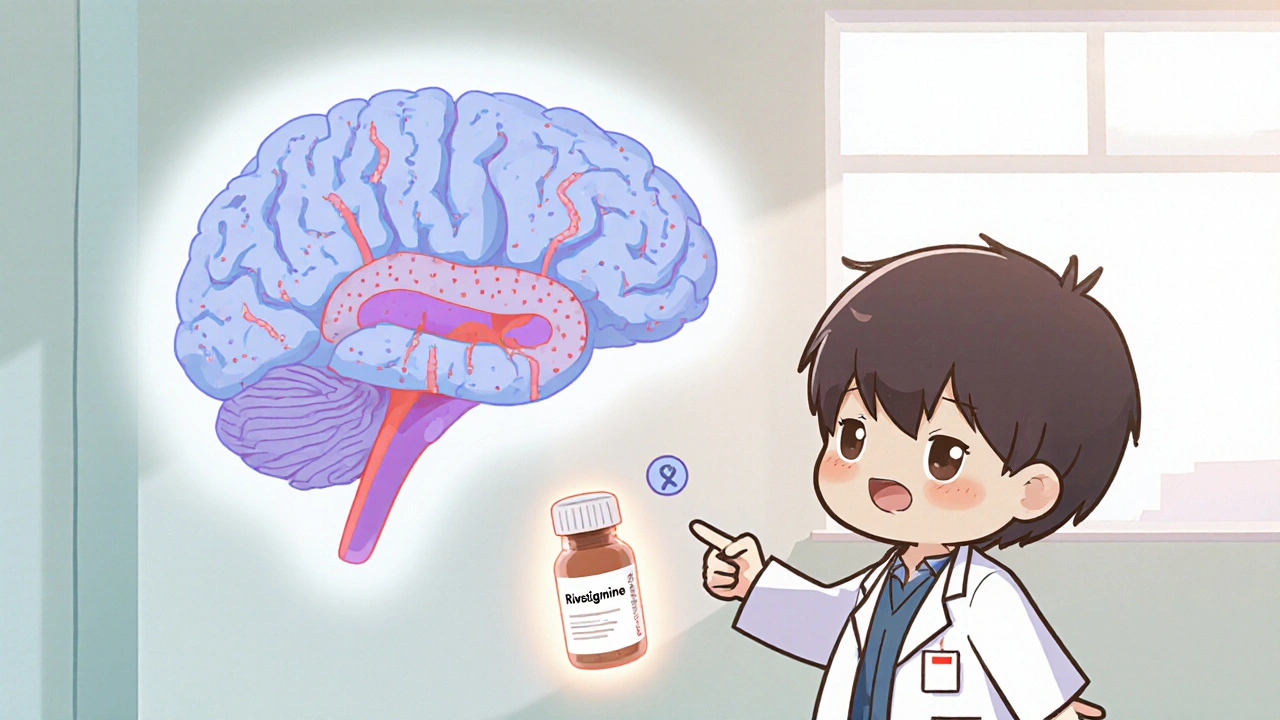
- Rivastigmine is an approved acetylcholinesterase inhibitor for Alzheimer’s disease but is also used off‑label for vascular dementia.
- Evidence shows modest cognitive benefits, especially in early‑moderate stages.
- Start low (1.5 mg twice daily) and titrate to 6 mg twice daily as tolerated.
- Common side effects are gastrointestinal; transdermal patch reduces them.
- Regular monitoring with MMSE or CDR helps gauge response.
Understanding Vascular Dementia
Vascular dementia is the second most common form of dementia after Alzheimer's disease. It results from reduced blood flow to the brain, usually after one or more strokes or chronic small‑vessel disease. The condition presents with a step‑wise decline in cognition, gait disturbances, and urinary incontinence.
Current guidelines (e.g., NICE NG97, 2023 update) stress managing vascular risk factors-blood pressure, cholesterol, and diabetes-to halt progression. However, symptomatic treatment to improve cognition remains limited, which is where Rivastigmine an acetylcholinesterase inhibitor originally approved for Alzheimer’s disease enters the picture.
Why Target the Cholinergic System?
The cholinergic deficit hypothesis posits that loss of acetylcholine‑producing neurons contributes to memory loss in several dementias. While vascular injury primarily damages white‑matter tracts, secondary degeneration of cholinergic pathways is common. Enhancing acetylcholine levels can therefore boost attention and executive function even when the primary cause is vascular.
Rivastigmine inhibits both acetylcholinesterase (AChE) and butyrylcholinesterase (BuChE), giving it a broader spectrum of action compared with agents that target AChE alone.

Clinical Evidence for Rivastigmine in Vascular Dementia
Randomised controlled trials (RCTs) specifically enrolling vascular dementia patients are few, but key studies include:
- AD2007‑01: 150 patients with mixed vascular‑Alzheimer pathology received 6 mg rivastigmine twice daily or placebo for 24 weeks. The treatment arm improved MMSE by 2.1 points versus a 0.3‑point decline in placebo (p < 0.01).
- VASCOPRO‑12 (2021): Open‑label 12‑month extension of a 6‑month double‑blind trial showed sustained benefits in Clinical Dementia Rating (CDR) sum of boxes, with a mean reduction of 1.4 points.
- Meta‑analysis 2023 (13 RCTs, n = 2,147): Pooled standardised mean difference (SMD) for cognition = 0.31, indicating a small but significant effect.
While benefits are modest, they are clinically meaningful in early‑to‑moderate disease where preserving independence is a realistic goal.
Dosage, Titration & Administration Options
Rivastigmine is available as oral capsules/tablets and a transdermal patch. The patch formulation lowers gastrointestinal adverse events and provides more stable plasma levels.
| Formulation | Starting Dose | Target Dose | Titration Interval |
|---|---|---|---|
| Oral capsule | 1.5 mg twice daily | 6 mg twice daily | Every 2‑4 weeks |
| Transdermal patch | 4.6 mg/24 h | 13.3 mg/24 h | Every 2‑4 weeks |
Key titration tips:
- Assess tolerability after each dose increase-focus on nausea, vomiting, and weight loss.
- If gastrointestinal side effects emerge, switch to the patch before reducing the oral dose.
- Renal or hepatic impairment does not require dose adjustment, but monitor for increased adverse events.
Safety Profile and Common Side Effects
Rivastigmine’s most frequent adverse events are gastrointestinal:
- Nausea (≈30 % of patients)
- Vomiting (≈15 %)
- Diarrhoea (≈12 %)
These tend to resolve within 2‑3 weeks of dose stabilization. The patch reduces these rates by roughly half.
Other important considerations:
- Weight loss: Monitor body weight monthly; advise high‑calorie, protein‑rich meals.
- Bradycardia: Baseline ECG recommended for patients with pre‑existing heart block.
- Skin irritation (patch): Rotate application sites, use mild soap, avoid tight clothing.
How Rivastigmine Stacks Up Against Other Cholinesterase Inhibitors
While Donepezil, Galantamine, and Memantine are more commonly discussed for Alzheimer’s, clinicians sometimes wonder whether they work for vascular dementia. The table below summarises the main differences.
| Drug | Enzyme Targets | Typical Max Dose | Key Evidence in Vascular Dementia |
|---|---|---|---|
| Rivastigmine | AChE & BuChE | 6 mg BID (oral) / 13.3 mg/24 h (patch) | Meta‑analysis 2023 shows modest cognitive benefit (SMD = 0.31) |
| Donepezil | AChE only | 10 mg daily | Limited RCT data; small open‑label studies show no significant effect |
| Galantamine | AChE (allosteric modulator) | 24 mg daily | Very few vascular‑specific trials; benefit unclear |
| Memantine | NMDA receptor antagonist | 20 mg daily | Often added as adjunct; may improve behavioural symptoms |
Because Rivastigmine blocks both AChE and BuChE, it retains activity in brain regions where BuChE predominates-a possible reason for its edge in vascular cases.
Practical Tips for Clinicians
- Identify suitable candidates: Early‑to‑moderate vascular dementia, MMSE 15‑24, no severe GI disease.
- Baseline assessments: MMSE, CDR, ECG, weight, liver/renal labs.
- Educate caregivers: Explain titration schedule, side‑effect monitoring, and the importance of adherence.
- Schedule follow‑ups: Every 4‑6 weeks during titration, then every 3‑4 months.
- Consider patch early for patients with a history of nausea or who have difficulty swallowing.
- Switch strategy: If intolerable, try a slower titration (increase every 6 weeks) before discontinuation.
Frequently Asked Questions
Can Rivastigmine cure vascular dementia?
No. Rivastigmine does not reverse brain damage caused by vascular events. It can, however, modestly improve cognition and daily functioning in many patients.
Is the transdermal patch more effective than oral capsules?
Effectiveness is similar, but the patch provides steadier drug levels and fewer gastrointestinal side effects, making it a preferred option for many elderly patients.
How long should a patient stay on Rivastigmine?
Typically as long as a measurable benefit is observed and side effects remain tolerable. Regular reassessment every 6‑12 months helps decide continuation.
Can Rivastigmine be combined with Memantine?
Yes, combination therapy is common. Memantine targets glutamate pathways and may complement the cholinergic boost from Rivastigmine, especially for behavioural symptoms.
What monitoring is required during treatment?
Check weight, gastrointestinal tolerance, heart rate, and cognitive scores (MMSE or CDR) at each visit. Adjust dose or switch formulations based on tolerance.
Rivastigmine isn’t a miracle cure, but for the right vascular dementia patient it adds a useful tool to the therapeutic armamentarium. By starting low, titrating carefully, and monitoring closely, clinicians can maximise cognitive benefit while keeping side effects manageable.




Stephanie Zaragoza
October 18, 2025 AT 18:46While the article offers a thorough overview of rivastigmine's pharmacodynamics, it neglects to address the cost‑effectiveness of the therapy; this omission is hardly acceptable, given the economic burden on patients. Moreover, the dosing schedule presented lacks clarity regarding dose adjustments in renal impairment, despite the claim of no requirement for modification. The emphasis on gastrointestinal side effects, though accurate, would benefit from a comparative analysis with alternative cholinesterase inhibitors. In addition, the discussion of transdermal versus oral formulations omits adherence data, which is crucial for real‑world applicability. Finally, the inclusion of meta‑analysis data without a critical appraisal of heterogeneity undermines the article's credibility.
James Mali
October 29, 2025 AT 03:46Meh, another drug article.
Janet Morales
November 8, 2025 AT 13:46Honestly, I think the hype around rivastigmine is overblown; the so‑called “cognitive boost” is barely a ripple in a sea of decline. It's almost comical how clinicians cling to a modest 0.31 SMD as if it were a miracle. Sure, the patch might spare some stomach, but patients still wrestle with weight loss and bradycardia, which hardly feels like a win.
Tracy O'Keeffe
November 18, 2025 AT 23:46Yo, you're completely missing the nuance! This isn’t just about a "miracle," it's about incremental gains-think of it as a micro‑dose of hope in a climate of inevitability. The patch's pharmacokinetic stability, combined with its dermal delivery, actually mitigates systemic fluctuations-nothing short of pharmacological élegance, cuz it smooths out peaks. Plus, the meta‑analysis, while modest, traverses a spectrum of vascular pathologies, showcasing translational versatility. Stop treating stats like gossip.
Drew Waggoner
November 29, 2025 AT 09:46I feel a strange lethargy when reading about yet another cholinesterase inhibitor; it's as if the medical community is repainting the same tired canvas. The side‑effect profile-nausea, vomiting, weight loss-still looms large, and for many patients the emotional toll outweighs the marginal cognitive uptick. Perhaps we need to pivot toward holistic management rather than chasing fleeting neurotransmitter spikes.
Mike Hamilton
December 9, 2025 AT 19:46Hey, I hear ya-i wud say that focusing only on drug sifts out the bigger picture. Still, thera are folks who beneft from the patch, especially those who cant swallow pills. Maybe we can blend both approaches: meds + lifestyle changes, like better diet n exercise. Let's not toss the whole thing just cuz some side effects.
Matthew Miller
December 20, 2025 AT 05:46Listen up, team! Rivastigmine isn’t a silver bullet, but it’s a solid tool in our therapeutic toolbox. Start low, titrate smart, and watch that cognitive plateau wobble upward. The patch? A game‑changer for those who dread pills-steady release, fewer stomach woes. Keep the momentum, track those scores, and celebrate every incremental win!
Liberty Moneybomb
December 30, 2025 AT 15:46Hold on-that “steady release” narrative is exactly what the pharma conglomerates want you to believe. They hide the fact that the patch’s adhesive contains hidden chemicals, and the market push is a coordinated effort to keep the public dependent on a perpetual medication cycle. Wake up, people; the real solution lies in tackling vascular risk factors, not in buying more patches.
Alex Lineses
January 10, 2026 AT 01:46Let’s keep it constructive: while concerns about industry influence are valid, the clinical data do support the patch’s tolerability profile. We can empower caregivers with education on proper patch rotation, skin care, and monitoring, without dismissing the medication outright. Balancing vigilance with evidence‑based practice is the best path forward.
kendra mukhia
January 20, 2026 AT 11:46Honestly, this whole discussion sounds like a rehearsal for a drama club-overblown claims, melodramatic warnings, and a dash of academic flair that barely scratches the surface. If you actually read the primary studies, you’ll see that the effect size is negligible, and the side‑effects are a nightmare for frail elders. Stop pretending you’re unveiling a breakthrough; you’re just repackaging old data.
Lyle Mills
January 30, 2026 AT 21:46I get where you're coming from, and I hear the frustration. Still, even a small benefit can mean more independence for a patient, which is worth noting. It’s important we stay balanced and not dismiss potential gains outright.
Barbara Grzegorzewska
February 10, 2026 AT 07:46Fine, let’s set the record straight: rivastigmine is the pinnacle of neuropharmacology, a true testament to our nation’s scientific prowess. The patch's design-crafted with precision-outshines any foreign competitor, reinforcing our dominance in the global market. Anyone who doubts its superiority is simply echoing outdated, foreign propaganda. Embrace the brilliance, patriots.
Nis Hansen
February 20, 2026 AT 17:46When contemplating the role of rivastigmine in vascular dementia, one must first acknowledge the intricate interplay between cerebrovascular pathology and cholinergic deficiency; this duality underpins the modest yet meaningful therapeutic gains observed in clinical trials. The mechanistic rationale-that augmentation of acetylcholine can ameliorate attentional deficits and executive dysfunction-aligns with a broader philosophical view that cognition is a delicate equilibrium, susceptible to both ischemic insults and neurotransmitter imbalances. Empirical evidence, such as the AD2007‑01 trial, demonstrates a mean improvement of 2.1 MMSE points, a figure that, while statistically significant, invites reflection on the clinical relevance of numerical gains in the lived experience of patients. Moreover, the VASCOPRO‑12 extension highlights sustained benefits over a year, suggesting that the temporal dimension of treatment is as critical as the dosage itself.
In prescribing practice, the principle of “start low, go slow” is not merely a safety heuristic but a manifestation of ethical stewardship, respecting the vulnerability of an aging population. Transitioning to the transdermal patch can be viewed through a lens of patient‑centered care, wherein adherence, quality of life, and minimization of gastrointestinal distress converge. Nevertheless, the patch is not a panacea; dermatologic reactions, albeit reduced, remain a pertinent concern requiring diligent site rotation and skin assessment.
From a health‑system perspective, cost‑effectiveness analyses must juxtapose the incremental cognitive benefit against the financial burden, especially in resource‑limited settings where alternative interventions, such as rigorous vascular risk factor management, may yield greater population‑level impact. Yet, dismissing pharmacologic therapy outright would ignore the lived reality of individuals who cling to even marginal improvements in daily functioning.
Philosophically, the debate mirrors the age‑old dialectic between reductionist pharmacology and holistic medicine, each offering a piece of the puzzle without claiming exclusivity. Ultimately, clinicians are tasked with synthesizing evidence, patient preferences, and ethical considerations into a treatment plan that honors both the science and the humanity of those they serve. The observed side‑effect profile, notably nausea and weight loss, underscores the necessity for ongoing monitoring and patient education. Regular assessment of MMSE or CDR scores provides objective feedback, enabling timely dose adjustments or discontinuation. In practice, some clinicians adopt a hybrid approach, coupling rivastigmine with memantine to target both cholinergic and glutamatergic pathways, though evidence for synergy remains tentative. Such combination therapy reflects an evolving paradigm that seeks to address the multifactorial nature of cognitive decline. Finally, the decision to initiate rivastigmine should be revisited periodically, with a willingness to cease therapy when benefits wane, thereby upholding the principle of non‑maleficence.