Formulary Tiers: How Insurance Plans Control Your Drug Costs
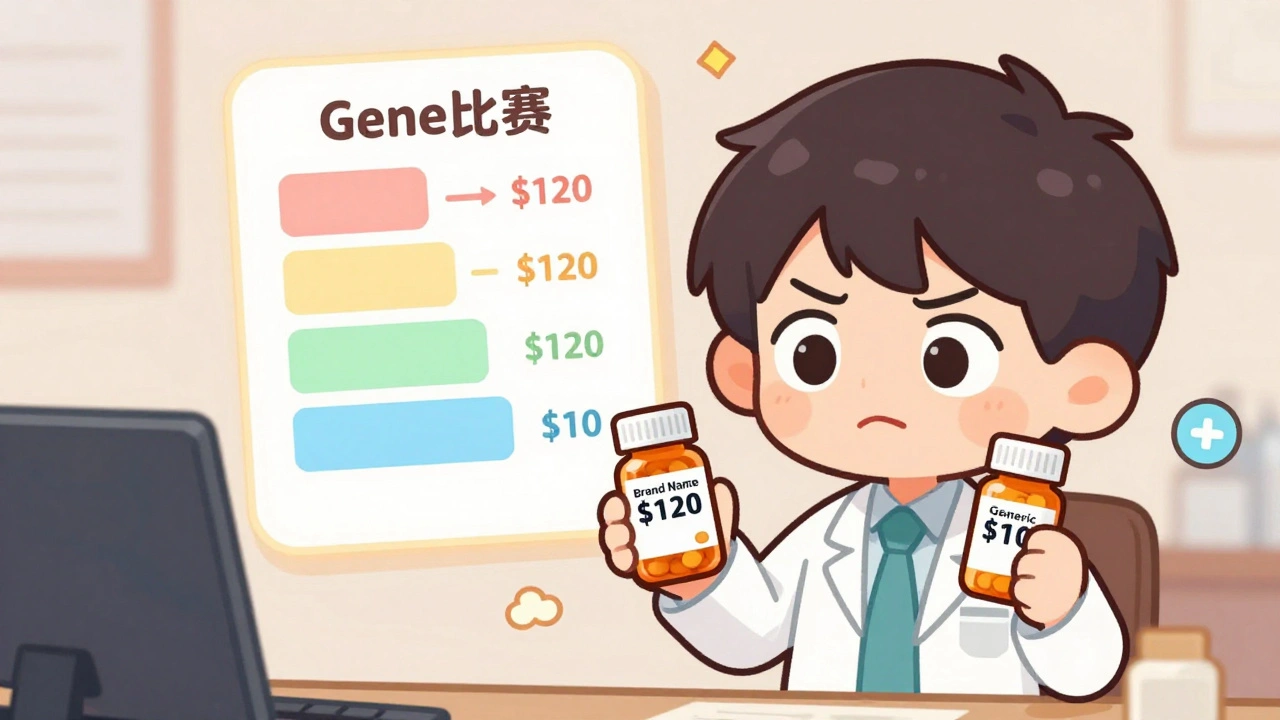
When your pharmacy says your prescription is formulary tiers, a system insurance companies use to organize drugs by cost and coverage. Also known as drug tiers, it’s not just a list—it’s a gatekeeper that decides whether you pay $5, $50, or $500 for the same medicine. Every drug your insurer covers gets slapped into one of these tiers, and where it lands changes everything: your out-of-pocket cost, whether you need prior approval, or if you’re even allowed to get it at all.
Prior authorization, a hurdle insurers force you to jump before they’ll pay, often shows up with higher-tier drugs like specialty biologics or even some generics. Meanwhile, step therapy forces you to try cheaper drugs first—even if your doctor says they won’t work for you. These aren’t random rules. They’re designed to push you toward the cheapest option, not the best one. And that’s why so many people end up fighting denials for generic medications they’ve used safely for years.
Formulary tiers don’t care about your medical history. They care about price tags and rebates. A drug might be clinically identical to another, but if the manufacturer pays the insurer a bigger kickback, it gets moved to Tier 1. Meanwhile, a drug your doctor swears by? If it’s on Tier 4 or 5, you’re looking at hundreds a month—even if it’s a generic. That’s why posts on this page dive into real cases: people who had to appeal insurance denials, patients who discovered manufacturing defects in their low-cost generics, and others who learned how to check if their meds were recalled by lot number. You’ll find guides on how Medicaid handles formularies in 2025, how Australia keeps drugs affordable with reference pricing, and why some doctors write "Do Not Substitute" on prescriptions.
This isn’t about confusing jargon. It’s about power. Who controls your access to medicine? Your doctor? Or an algorithm in an insurance company’s back office? The posts here cut through the noise. You’ll learn how to read your plan’s formulary, when to push back, how to get exceptions, and what to do when your pharmacy says "it’s not covered"—even when it should be. You’ll see how temperature control, pill organizers, and medication reconciliation all tie into this system. Because if your drug isn’t on the right tier, none of the safety tips matter. You won’t even get to the pharmacy.
Employer Health Plans and Generic Drugs: How Formularies Control Your Prescription Costs
Learn how employer health plans use formularies to control prescription costs, why generics are your best bet, and what to do when your drug gets removed from coverage.
read more



