When a medication changes your heart’s electrical rhythm in ways you can’t feel, it’s not just a side effect-it’s a silent danger. QT prolongation is one of those hidden risks that doesn’t cause symptoms until it’s too late. It shows up on an ECG as a longer-than-normal QT interval, meaning your heart’s ventricles are taking too long to recharge between beats. That delay can trigger a deadly arrhythmia called torsades de pointes, which can spiral into sudden cardiac arrest. And here’s the thing: it’s not rare. Over 200 medications, from antibiotics to antidepressants, are known to cause it.
What Exactly Is QT Prolongation?
The QT interval on an ECG measures how long it takes your heart’s lower chambers to contract and reset. It’s not a fixed number-it changes with your heart rate. That’s why doctors use a corrected version, called QTc. A normal QTc is under 450 ms for men and 460 ms for women. Once it crosses 500 ms, the risk of torsades de pointes jumps 3 to 5 times. Even a rise of more than 60 ms from your baseline can be dangerous. This isn’t just theoretical. In the U.S., over 200 drugs have been flagged by crediblemeds.org for their potential to cause this. Many of them are commonly prescribed.
Which Medications Are the Biggest Culprits?
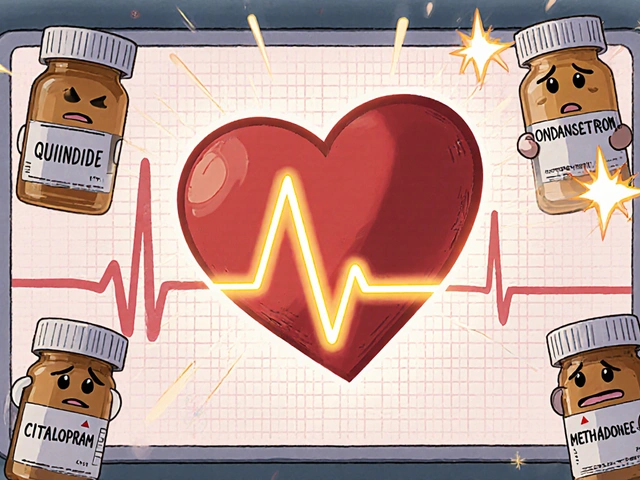
Not all QT-prolonging drugs are created equal. Some are designed to affect heart rhythm, others do it by accident. The highest-risk group includes Class Ia and Class III antiarrhythmics like quinidine, sotalol, and dofetilide. Sotalol, for example, can increase QTc by 10-40 ms depending on the dose-and about 2-5% of patients on it develop torsades. Quinidine causes it in up to 6% of users.
But you don’t need a heart drug to be at risk. Common antibiotics like erythromycin and clarithromycin can prolong QT by 15-25 ms, especially when taken with other drugs that slow their breakdown. Antifungals like fluconazole and even the popular anti-nausea drug ondansetron have been linked to cases of torsades. Antipsychotics like haloperidol and ziprasidone carry black box warnings for this exact reason. And then there’s citalopram: the FDA capped its maximum daily dose at 40 mg (20 mg for people over 60) because higher doses reliably stretch the QT interval.
Methadone is another silent threat. At doses over 100 mg per day, it’s strongly associated with torsades. Even though it’s used safely in thousands for opioid addiction, it demands strict ECG monitoring. The same goes for newer cancer drugs like vandetanib and nilotinib, which are now known to prolong QT in over 40% of cases.
Why Are Some People at Higher Risk?
It’s not just about the drug. It’s about the person. Women make up about 70% of documented torsades cases. Why? Their hearts naturally have longer repolarization times, and hormonal shifts-like after childbirth-make them even more vulnerable. Age matters too. People over 65 are at higher risk, partly because they often take multiple medications and have reduced kidney or liver function, which slows drug clearance.
Low potassium, low magnesium, or low calcium levels can make QT prolongation worse. That’s why people on diuretics or with eating disorders are at greater risk. Genetics play a role too. About 30% of drug-induced torsades cases happen in people with subtle, undiagnosed mutations in the hERG gene, which controls the potassium channel that most of these drugs block. You might never know you’re at risk until a medication triggers a crisis.
And here’s the most dangerous part: combining drugs. Taking two QT-prolonging medications together doesn’t just add risk-it multiplies it. A 2020 FDA review found that 68% of torsades cases involved two or more such drugs. Common dangerous combos? Ondansetron + azithromycin. Haloperidol + citalopram. Erythromycin + fluconazole. These aren’t rare mix-ups. They happen in emergency rooms, hospitals, and even primary care offices.
How Is It Detected and Monitored?
There’s no blood test for QT prolongation. It’s all about the ECG. But reading an ECG isn’t simple. The most common way to correct for heart rate is Bazett’s formula, but it’s inaccurate at very slow or fast rates. Many clinicians still get it wrong. That’s why hospitals are starting to use automated ECG systems with built-in QTc alerts. A 2022 study showed these systems cut inappropriate prescribing by 58%.
Guidelines from the European Society of Cardiology and the American Heart Association now recommend a baseline ECG before starting high-risk drugs-especially if you’re over 65, have heart disease, or are taking more than one QT-prolonging medication. A follow-up ECG within 3 to 7 days is often needed after a dose increase. If QTc hits 500 ms or rises more than 60 ms from baseline, the drug should be stopped unless there’s no alternative.
For patients on long-term drugs like methadone or amiodarone, quarterly ECGs are standard. But many clinics still don’t do this. A 2022 survey of hospital pharmacists found that 63% felt unsure how to safely combine these drugs. That’s not just a knowledge gap-it’s a patient safety gap.
What’s Changing in Drug Safety?
For years, drug companies only had to test whether a new medicine prolonged the QT interval. That’s no longer enough. Since 2013, the FDA, EMA, and other global regulators have been using a new system called CiPA (Comprehensive in vitro Proarrhythmia Assay). It doesn’t just look at one potassium channel-it tests how a drug affects multiple ion channels and uses computer models to predict real-world arrhythmia risk.
The result? More drugs are being dropped in late-stage trials. Between 2016 and 2022, 22 drugs were abandoned because of proarrhythmia risk. Each failure cost over $2.6 billion. But it’s saving lives. Newer drugs like retatrutide, approved in late 2023 for obesity, were flagged early for QT prolongation (8.2 ms increase) and are now labeled with clear warnings.
Future tools are even more promising. In 2024, researchers developed an AI algorithm that predicts torsades risk with 89% accuracy by analyzing tiny, invisible patterns in ECG waveforms-not just the QT interval. This could one day replace manual readings in emergency rooms and clinics.
What Should You Do?
If you’re on any medication, especially one listed above, ask your doctor or pharmacist: "Could this affect my heart rhythm?" If you’re on multiple meds, ask: "Could any of these interact to raise my risk?" If you’re over 65, female, or have heart disease, insist on a baseline ECG before starting a new drug.
Don’t wait for symptoms. Torsades often strikes without warning. If you’ve ever had unexplained fainting, dizziness, or palpitations after starting a new drug, get an ECG. Even if you feel fine, a simple 10-second test could prevent a cardiac arrest.
And if you’re a healthcare provider: don’t rely on memory. Use crediblemeds.org. Check your ECG software settings. Know your patient’s electrolytes. Avoid unnecessary combos. The tools are there. The data is clear. What’s missing is consistent action.
What Happens If It’s Not Caught?
One case of torsades can cost a hospital nearly $39,000. But the real cost is human. Many patients don’t survive. Others live with permanent brain damage from lack of oxygen during cardiac arrest. The good news? These deaths are preventable. Systematic screening and better prescribing have already reduced drug-induced torsades by 40% over the last decade. We know how to stop it. Now we just need to do it consistently.
Can a normal ECG rule out QT prolongation risk?
No. A normal ECG doesn’t mean you’re safe. QT prolongation can develop days after starting a drug, especially with long-acting medications like amiodarone or methadone. A single baseline ECG is just the start. Repeat monitoring after dose changes or when adding other drugs is essential. Risk isn’t static-it changes with your body, your meds, and your health.
Are over-the-counter drugs safe for QT prolongation?
Some aren’t. Antihistamines like diphenhydramine (Benadryl) and certain cough syrups containing dextromethorphan can prolong QT, especially in high doses or when mixed with other drugs. Even herbal supplements like licorice root can lower potassium and indirectly increase risk. Just because something is sold without a prescription doesn’t mean it’s safe for your heart.
Is QT prolongation always permanent?
Usually not. If caught early and the offending drug is stopped, the QT interval often returns to normal within days to weeks. But if torsades occurs and isn’t treated immediately, it can lead to sudden death. The key is early detection and prompt action-not waiting for symptoms.
Can I still take my antidepressant if I have QT prolongation?
It depends. Citalopram and escitalopram have clear dose limits because of QT risk. Other antidepressants like sertraline or bupropion have minimal QT effects and are safer choices. Never stop an antidepressant abruptly. Talk to your doctor about switching to a lower-risk option if your QTc is elevated. Your mental health matters-but so does your heart.
How often should I get an ECG if I’m on a QT-prolonging drug?
For high-risk drugs like sotalol, dofetilide, or methadone, get a baseline ECG before starting, then repeat within 3-7 days after initiation or any dose increase. For long-term use, quarterly ECGs are recommended. If you’re on multiple QT-prolonging drugs or have other risk factors (age, low electrolytes, heart disease), your doctor may want even more frequent monitoring. Don’t assume one ECG is enough.






Jeremy Samuel
November 20, 2025 AT 06:39Destiny Annamaria
November 22, 2025 AT 02:44Matthew Karrs
November 23, 2025 AT 04:31Alyssa Torres
November 23, 2025 AT 19:07Summer Joy
November 23, 2025 AT 21:40Dana Oralkhan
November 24, 2025 AT 16:55Nicole Ziegler
November 25, 2025 AT 03:59Ron and Gill Day
November 26, 2025 AT 19:09Aruna Urban Planner
November 28, 2025 AT 14:18Kristi Bennardo
November 28, 2025 AT 15:00Bharat Alasandi
November 28, 2025 AT 16:04