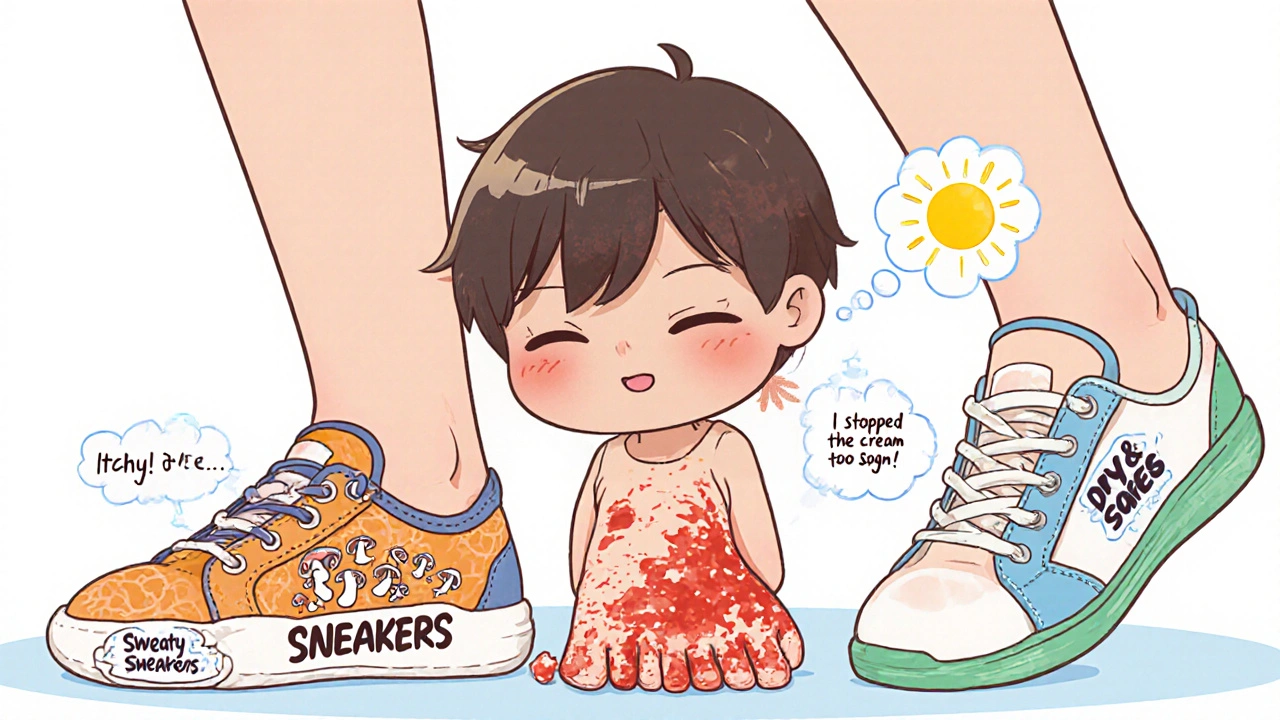
Most people think fungal infections are just annoying rashes or itchy feet. But if you’ve had one, you know they don’t go away on their own. And they don’t just disappear after a few days of cream. Fungal infections are sneaky. They come back. They spread. And if you ignore them, they can turn into something worse - especially if you have diabetes, a weak immune system, or just keep wearing damp socks.
What’s Really Causing Your Itch?
Not all fungal infections are the same. Two of the most common types - athlete’s foot and Candida - are caused by completely different fungi, and they need different treatments.Athlete’s foot, also called tinea pedis, is caused by dermatophytes. These are fungi that eat keratin - the tough protein in your skin, hair, and nails. That’s why they love your feet. Warm, sweaty shoes? Perfect. Locker rooms, public showers, pool decks? They’re basically fungal hotels. The most common culprit is Trichophyton rubrum. It doesn’t just sit there. It spreads. And if you scratch, you can move it to your hands, groin, or even under your nails.
Candida, on the other hand, is a yeast. Candida albicans is the usual suspect. It lives in your mouth, gut, and vagina naturally - in small amounts. But when your body’s balance gets thrown off - by antibiotics, diabetes, pregnancy, or a weakened immune system - it overgrows. That’s when you get thrush, vaginal yeast infections, or skin folds that turn red and sore. Unlike athlete’s foot, Candida doesn’t need keratin to survive. It can grow on moist, non-keratinized skin too - like between your toes, under your breasts, or in your mouth.
How Do You Know Which One You Have?
It’s easy to mix them up. Both cause itching, redness, and flaking. But here’s how to tell the difference:- Athlete’s foot: Starts between your toes - especially the fourth and fifth. Skin peels, cracks, or turns white and soggy. Sometimes it spreads to the soles of your feet in a "moccasin" pattern - dry, scaly skin that looks like you’ve been wearing rough shoes all winter. Blisters? That’s the less common "vesicular" type.
- Candida infection: Bright red, shiny patches. Often with small pustules around the edges. In the groin, it’s called jock itch. In the mouth, it’s white patches that scrape off (thrush). Vaginal yeast infections bring thick, white discharge and intense burning.
One big clue? Athlete’s foot usually doesn’t hurt unless it gets infected with bacteria. Candida infections often burn more than they itch. And if you’ve had a yeast infection before, you’ll recognize the feeling.
What Treatments Actually Work?
Not all antifungal creams are created equal. And not all of them work fast - or at all.For mild athlete’s foot, over-the-counter creams like clotrimazole or miconazole are fine. But here’s the catch: you have to use them long enough. Most people stop when the itching stops. That’s a mistake. Fungi are still there. That’s why 40% of cases come back within a year.
Studies show that terbinafine (Lamisil) works better. It kills the fungus, not just slows it down. One user on Reddit said their six-month case cleared up in 10 days after clotrimazole failed for weeks. That’s not luck. Terbinafine has a 70-90% cure rate when used correctly.
For stubborn cases - especially if the skin is cracked or thickened - Whitfield’s ointment (a mix of salicylic acid and benzoic acid) helps. It doesn’t kill the fungus directly. Instead, it peels away the dead, infected skin so the antifungal can reach deeper. One study found it cleared 65% of interdigital cases at four weeks, compared to 55% for clotrimazole alone.
Oral meds like terbinafine (250 mg daily for 2-6 weeks) or itraconazole are reserved for severe or recurring cases. They’re more effective because they get into the skin from the inside out. But they’re not for everyone. Liver checks are needed before starting. And they cost more.
For Candida, fluconazole (a single 150 mg pill) often clears up vaginal yeast infections in one dose. Topical creams like clotrimazole work too, but oral treatment is faster and more reliable for recurrent cases. In 2021, the FDA approved ibrexafungerp - the first new class of antifungal in 20 years - for stubborn vaginal yeast infections that didn’t respond to older drugs.

Why Do These Infections Keep Coming Back?
Because most people treat the symptom, not the cause.You use the cream. The itching stops. You stop using it. Three weeks later, it’s back. That’s because the fungus is still hiding - in your shoes, under your toenails, in the cracks of your bathroom floor.
Here’s what really works to stop recurrence:
- Change your socks daily. Cotton or moisture-wicking blends. No synthetics.
- Wear flip-flops in public showers, pools, and gyms.
- Let your feet breathe. Avoid tight shoes. Rotate your footwear so they dry out completely between uses.
- Use antifungal powder in your shoes and socks. Even after the infection clears. Miconazole powder (2%) is cheap and effective.
- Wash your towels, sheets, and socks in hot water. Fungi survive on fabric.
- Keep your skin dry. After showering, pat between your toes - don’t rub. Use a hairdryer on cool if needed.
People with diabetes are at higher risk. High blood sugar feeds fungi. And poor circulation means your body can’t fight the infection well. That’s why the CDC’s "My Action Plan" program - which teaches diabetic patients daily foot checks and hygiene - reduced recurrent infections by 35% in clinics that used it.
When Should You See a Doctor?
You don’t need to run to the clinic for a mild rash. But if any of these happen, get help:- Your skin is swollen, hot, or oozing pus - that’s a bacterial infection on top of the fungus. You’ll need antibiotics.
- The infection spreads to your nails (they turn yellow, thick, and crumbly). That’s onychomycosis. It needs oral meds.
- You have diabetes or a weakened immune system. Even a small foot rash can turn into cellulitis - a dangerous skin infection.
- You’ve tried two different antifungals for four weeks with no improvement.
- You keep getting yeast infections (four or more a year). That’s not normal. You might have undiagnosed diabetes or another underlying issue.
And don’t ignore nail infections. They’re harder to treat. Topical creams rarely reach deep enough. Oral antifungals are the standard - but they take months. And they’re not always successful. New drugs like olorofim are in trials and show promise for resistant strains, but they’re not available yet.

What’s New in the Fight Against Fungi?
The good news? Science is catching up.Antifungal resistance is rising. A new strain of athlete’s foot fungus - Trichophyton indotineae - first spotted in India in 2017, has now spread to 28 countries. It doesn’t respond to terbinafine in up to 30% of cases. That’s why the WHO added it to its list of priority fungal pathogens.
Researchers are working on new treatments. Olorofim, a topical drug in Phase II trials, cleared 82% of stubborn athlete’s foot cases in 2023. And scientists are exploring vaccines and combination therapies to outsmart resistant strains.
But until then, the best defense is still simple: keep your skin dry, treat infections fully, and don’t wait until it’s too late.
What Not to Do
There are myths everywhere. Don’t fall for them:- "Hydrogen peroxide or vinegar will cure it." They might sting, but they don’t kill the fungus deep in your skin. And vinegar can irritate broken skin.
- "I’ll just use the same cream for my athlete’s foot and my yeast infection." Not always safe. Some creams aren’t formulated for mucous membranes.
- "It’s not contagious." It is. You can pick it up from floors, towels, or even your own dirty socks.
- "I’ll stop when it looks better." That’s the #1 reason it comes back.
And please - don’t scratch. You’ll spread it. You might break the skin. And then you’re not just dealing with a fungus. You’re dealing with bacteria too.
Can athlete’s foot spread to other parts of the body?
Yes. If you scratch your infected foot and then touch other areas - like your groin, hands, or underarms - you can transfer the fungus. That’s why jock itch and hand fungus often appear alongside athlete’s foot. Always wash your hands after touching the infected area, and avoid sharing towels or shoes.
How long does it take for antifungal cream to work?
You’ll usually feel relief from itching in 2-3 days. But the fungus isn’t gone. Most topical treatments need 2-4 weeks of daily use. Even after the skin looks normal, keep applying for another 1-2 weeks to make sure all the spores are dead. Stopping early is the main reason infections return.
Is athlete’s foot the same as ringworm?
Yes, technically. Both are caused by dermatophytes. Ringworm is just the name for fungal infections on the body, scalp, or nails. Athlete’s foot is ringworm on the feet. The same fungi can cause jock itch or nail infections. It’s all the same family of organisms - just in different places.
Can I use antifungal cream during pregnancy?
Most topical antifungals like clotrimazole and miconazole are considered safe during pregnancy for vaginal yeast infections and skin rashes. Oral fluconazole is usually avoided in the first trimester. Always check with your doctor before using any medication, even over-the-counter ones, while pregnant.
Do I need to throw away my shoes if I have athlete’s foot?
No, but you should treat them. Sprinkle antifungal powder inside each shoe daily for a few weeks. You can also use UV shoe sanitizers, which kill fungi effectively. If your shoes are old, smelly, or made of synthetic materials that trap moisture, consider replacing them. Fungi can live in shoes for months.
Why do some people keep getting yeast infections?
Frequent yeast infections (four or more a year) are a red flag. Common causes include uncontrolled diabetes, antibiotics, hormonal birth control, or a weakened immune system. If you’re getting them often, ask your doctor to test for diabetes or check your vaginal pH. Sometimes, long-term low-dose fluconazole or probiotics help prevent recurrence.
Final Thoughts
Fungal infections aren’t glamorous. They’re messy, persistent, and often embarrassing. But they’re also treatable - if you treat them right. Don’t rush. Don’t skip steps. Don’t ignore the signs. And don’t assume it’s just "a little itch." The same fungus that causes your peeling toes can lead to serious complications if you’re not careful.Keep your feet dry. Treat infections fully. And if it keeps coming back - see a doctor. It’s not weakness. It’s smart.





james lucas
November 24, 2025 AT 00:27man i thought i was the only one who kept getting athlete’s foot no matter how many creams i used
turned out my sneakers were the problem - they were just sitting in the closet for weeks
started using that miconazole powder like the post said and now my shoes dont smell like a locker room anymore
also switched to cotton socks and holy crap it’s been 8 months no return
seriously if you’re tired of this crap try the powder it’s like 5 bucks and works better than half the prescriptions i’ve paid for
Jessica Correa
November 25, 2025 AT 00:56i had a yeast infection last year and used fluconazole and it vanished in like two days
but then it came back two months later and i was like ok what now
turns out my birth control was making my sugar levels weird and my body was basically feeding the yeast
got tested for prediabetes and switched meds and now it’s been a year clean
so if you keep getting it dont just reach for the cream again
ask your doc to check your blood sugar its easier than you think
manish chaturvedi
November 25, 2025 AT 06:24as someone from India where Trichophyton indotineae is now common, i can confirm this is not a joke
my cousin tried terbinafine for six weeks and nothing happened
then he switched to oral itraconazole with topical Whitfield’s ointment and it cleared in three weeks
many doctors here still prescribe clotrimazole as first line - but that’s outdated
the new strain is resistant to terbinafine in nearly one in three cases
if you live in a humid climate or have traveled to South Asia recently, this is something to consider
do not underestimate fungal infections - they are not just "itchy feet"
they can become systemic in immunocompromised people
and yes, wearing flip-flops in public showers saves lives
Nikhil Chaurasia
November 27, 2025 AT 04:55i used to think fungal infections were a myth people made up to sell cream
until i got one after a hiking trip
it started as a tiny red spot between my toes
then it spread to my nails
then my hands
then my groin
and suddenly i was sitting in a dermatologist’s office with a prescription for 6 weeks of oral meds
and a lecture on how i ruined my life by wearing sweaty sneakers for 12 hours a day
now i shower, dry my feet like my life depends on it, and rotate shoes like they’re holy relics
and yes - i use antifungal powder even when i don’t have an infection
because i learned the hard way that fungi don’t care if you’re "clean"
they just want moisture and silence
Holly Schumacher
November 27, 2025 AT 13:26Why do people keep saying "use the cream for two weeks after symptoms disappear" when the entire medical literature says you need to treat for 4–6 weeks minimum for dermatophytes? It’s not a suggestion. It’s a biological imperative. You’re not "being careful" - you’re just delaying resistance. And don’t get me started on vinegar. Vinegar has a pH of 2.4. Your skin’s pH is 5.5. Pouring vinegar on broken skin is like pouring battery acid on a paper cut. And yet, every single Reddit thread has someone saying "my grandma used vinegar and it worked." No. It didn’t. It just made you feel better for 20 minutes while the fungus multiplied under the surface. Also, if you’re pregnant and using clotrimazole, you’re fine. But if you’re taking fluconazole orally without testing for liver enzymes, you’re playing Russian roulette with your hepatocytes. Stop self-diagnosing. Get a KOH prep. It takes five minutes. And if you’re still using the same socks from 2018 - just throw them out. They’re not "vintage." They’re fungal incubators.
Michael Fitzpatrick
November 28, 2025 AT 02:57man i used to think i was just bad at hygiene until i read this post
turns out i was just using the wrong cream
clotrimazole was doing nothing for me for months
then i grabbed terbinafine on sale and boom - gone in 10 days
and i’ve been using that antifungal powder in my shoes ever since
no more weird smells, no more peeling skin
and honestly? i feel like a new person
like i can walk barefoot in the house again without shame
and yeah i know it sounds silly
but when you’ve had this for years
it’s not just a rash
it’s your whole identity
you start avoiding beaches
you stop going to gyms
you stop wearing sandals
and then one day you try the right thing
and suddenly you’re walking around like you forgot you ever had a problem
it’s wild how something so small can change everything
Shawn Daughhetee
November 29, 2025 AT 16:21my dad had diabetes and he got a foot infection that turned into cellulitis
they had to hospitalize him for a week
he was on IV antibiotics and antifungals
they almost amputated his toe
after that he started checking his feet every night
and now he uses that powder in his shoes every morning
he’s 72 and still hikes
so if you think this isn’t serious
just talk to someone who almost lost a toe
it’s not about being neat
it’s about not ending up in the ER
and yeah i know you’re busy
but your feet don’t care how busy you are
they just want to stay dry
Miruna Alexandru
December 1, 2025 AT 00:16The entire premise of this post is dangerously reductive. You treat symptoms, not causes - but you don’t even mention the microbiome. Candida overgrowth isn’t just about antibiotics or sugar - it’s about dysbiosis, gut permeability, and chronic stress-induced cortisol elevation. The fact that you recommend fluconazole as a "fix" without addressing the root immune dysregulation is not just negligent - it’s complicit in perpetuating a cycle of recurrence. And your advice about socks? It’s surface-level. The real issue is systemic inflammation. If you’re getting recurrent yeast infections, your body is screaming for a low-glycemic, anti-inflammatory diet - not more antifungals. You’re treating the symptom, yes - but you’re ignoring the signal. And that’s why people keep coming back. Because you’re not healing them. You’re just temporarily suppressing them. The real cure? It’s not in a tube. It’s in your plate.
Patrick Marsh
December 1, 2025 AT 06:41Terbinafine works. Stop using clotrimazole if it’s been 2 weeks and no change.
Wash socks in hot water.
Don’t scratch.
Use powder.
See a doctor if it’s on your nails.
Done.
Daniel Jean-Baptiste
December 1, 2025 AT 21:34big up to the guy who mentioned whitfield’s ointment
i had a case that just wouldn’t quit
clotrimazole? nope
terbinafine? not enough
then i found whitfield’s at the drugstore next to the aspirin
used it for 3 weeks, scrubbed the dead skin off gently, then followed up with terbinafine
and boom - clean
also started wearing sandals at home
and i swear my feet feel lighter now
like they remember what air feels like
thanks for the real talk
most posts just say "use cream"
you actually told us how to win
New Yorkers
December 3, 2025 AT 06:45Let me guess - you’re from the suburbs. You think fungi are a "problem" because you’ve never lived in a city where the subway floors are literally covered in sweat and spores. You think washing socks fixes it? Try walking barefoot on a New York subway platform in July. Try sharing a shower with 12 people after a 10-hour shift. This isn’t about socks. It’s about class. It’s about who gets access to clean spaces, antifungal powders, and dermatologists. The real infection here? Inequality. The rest of you? You’re just scrubbing your feet while the system keeps feeding the fungus.
David Cunningham
December 3, 2025 AT 21:40just wanted to say - i’ve had athlete’s foot for 10 years
tried everything
even went to a naturopath who gave me tea tree oil and probiotics
nothing worked
then i found this post
terbinafine + antifungal powder + rotating shoes
three weeks later - no itch, no smell, no shame
now i wear sandals in winter just to feel the breeze on my toes
you’re right - it’s not glamorous
but it’s worth it
thanks for the real advice
not just the hype