Antihistamine Safety Calculator
Is Your Antihistamine Safe for Work?
This tool helps you determine if your antihistamine is safe for safety-sensitive jobs. Based on the FDA's latest guidelines and scientific evidence about medication safety.
Many people take antihistamines without thinking twice. They grab a pill for a runny nose, itchy eyes, or seasonal allergies, then head to work, get behind the wheel, or operate machinery. But what if that pill is silently slowing down your brain? The truth is, not all antihistamines are created equal-and the difference could mean the difference between getting home safely or ending up in an accident.
Why Some Antihistamines Make You Drowsy
First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine (Chlor-Trimeton), and hydroxyzine (Atarax) were developed decades ago to block histamine, the chemical your body releases during allergic reactions. But here’s the catch: they don’t stop at your nose or throat. These drugs are lipophilic, meaning they easily slip through the blood-brain barrier. Once inside, they interfere with histamine’s natural role in keeping you alert. Histamine isn’t just about sneezes-it’s a wake-up signal in your brain. When antihistamines block it, your brain slows down.What’s worse, you might not even feel it happening. A truck driver on Reddit shared how he took diphenhydramine for allergies and didn’t feel sleepy-but failed a roadside cognitive test. He couldn’t touch his nose with his finger. He wasn’t dozing off. His reaction time, coordination, and decision-making were already impaired. That’s the silent danger. Your brain thinks it’s fine. But your body isn’t performing like it should.
The Real Cost of Drowsiness at Work
Drowsiness from antihistamines isn’t just about nodding off at your desk. It affects precision, judgment, and speed. Studies show that first-generation antihistamines can reduce reaction time by 25-30% and increase lane deviation by 50% in driving simulators. That’s comparable to being legally drunk. In aviation, these drugs are the leading medication found in the toxicology reports of pilots who crashed. In construction, manufacturing, and healthcare, the risk is just as real. A nurse working night shifts switched from diphenhydramine to loratadine and noticed immediate improvement in alertness during procedures. She didn’t realize how much she’d been struggling until the fog lifted.And it’s not just driving. Falls are a major concern. More than one in four older adults fall each year, and first-generation antihistamines are a known contributor. For workers on ladders, forklifts, or assembly lines, even a momentary lapse in focus can lead to serious injury. The CDC and Care Partners CT both warn that these drugs increase fall risk-not because people feel dizzy, but because their motor control and balance are quietly compromised.

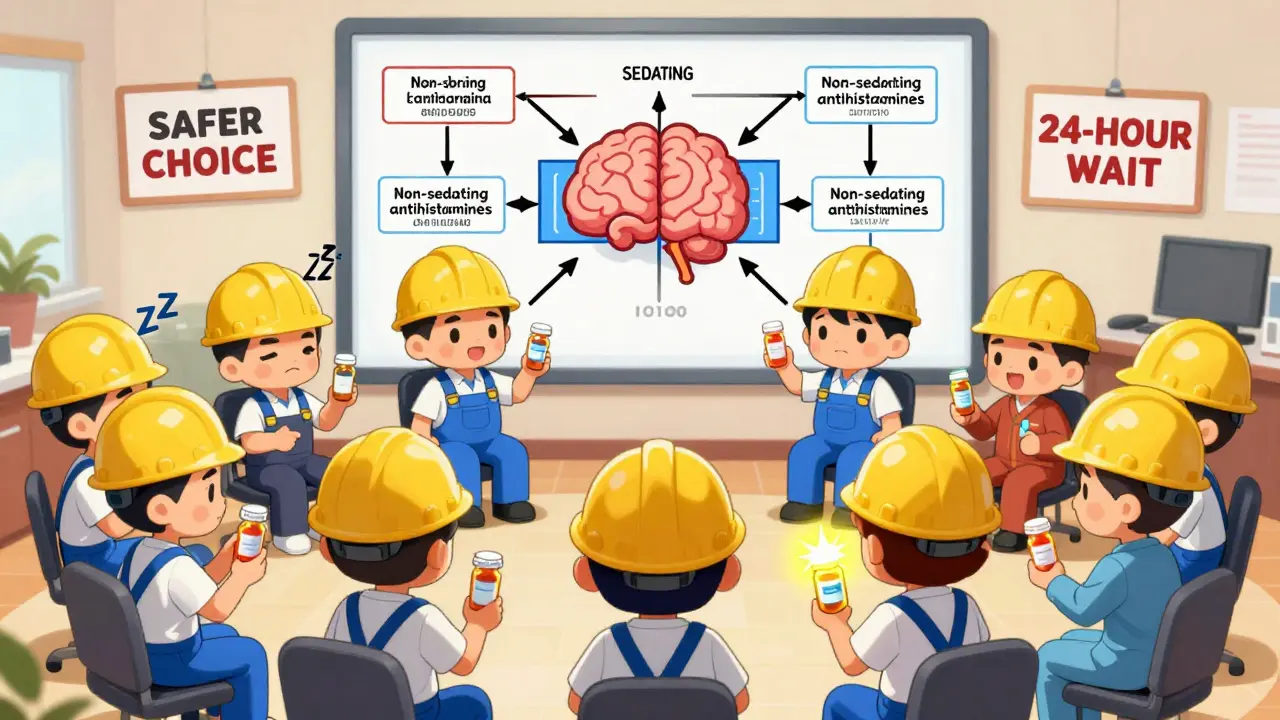
Second-Generation Antihistamines: The Safer Choice
Enter loratadine (Claritin), cetirizine (Zyrtec), fexofenadine (Allegra), and bilastine. These second-generation antihistamines were designed differently. Their chemical structure makes them poor at crossing the blood-brain barrier. They’re actively pumped out of the brain by P-glycoprotein transporters-your body’s natural defense system. The result? Minimal to no drowsiness.Studies confirm it. In psychometric tests and real-world driving simulations, second-generation antihistamines perform no worse than a placebo. On Healthgrades, 78% of Allegra users report no drowsiness. Only 12% of Benadryl users say the same. The difference isn’t subtle-it’s life-changing for anyone whose job requires attention to detail.
Even the half-life matters. First-generation antihistamines can linger in your system for 15 to 30 hours. That means if you take one at 8 a.m., you could still be impaired at 8 p.m. Second-generation options clear out in 8-12 hours. They’re also less likely to interact dangerously with alcohol or other sedatives. And unlike older drugs, their packaging now includes clearer warnings and timing advice-87% do, compared to just 43% of first-gen products.
Who’s at Risk? And What’s Being Done
It’s not just truck drivers and pilots. Nurses, factory workers, warehouse staff, emergency responders, and even office workers using heavy machinery or operating power tools are at risk. The National Highway Traffic Safety Administration estimates 100,000 police-reported crashes each year are caused by drowsiness-and that doesn’t include unreported ones. Antihistamines are a hidden contributor.Regulations are catching up. The FAA bans first-generation antihistamines for pilots. The Department of Transportation requires employers to include them in safety protocols. The European Medicines Agency issued warnings in 2019 for transport workers. In the U.S., the FDA updated labeling in March 2023 to make occupational risks harder to ignore. And companies are responding: 41% of Fortune 500 firms now include specific antihistamine guidance in their workplace health policies.
Healthcare professionals are changing too. A 2022 survey by the American Nurses Association found 73% of nurses now use only non-sedating antihistamines. That’s not just preference-it’s a safety standard.
What You Should Do
If you’re taking an antihistamine and your job involves driving, operating machinery, or any safety-sensitive task, here’s what you need to do:- Check the label. If it says “may cause drowsiness” or warns against operating machinery, it’s a first-generation drug.
- Switch to a second-generation option. Loratadine, cetirizine, and fexofenadine are widely available over the counter. Ask your pharmacist if you’re unsure.
- Test it first. Take a new antihistamine at home before work. See how you feel after 4-6 hours. Can you concentrate? Do your hands feel steady? If you’re even slightly off, don’t risk it.
- Wait 24 hours after first-gen use. Even if you feel fine, the drug may still be affecting you. The National Sleep Foundation recommends waiting a full day before returning to safety-sensitive duties.
- Never mix with alcohol or sedatives. The combination multiplies impairment. A drink and a Benadryl? That’s not a good night’s sleep-it’s a recipe for disaster.
There’s no shame in choosing safety over convenience. If you’ve been taking diphenhydramine because it’s cheap or you think it works better, you’re not alone. But the science is clear: the cost isn’t worth it. Your brain, your coworkers, and your family deserve better.
What Employers Should Know
If you manage a team in transportation, construction, healthcare, or manufacturing, your responsibility goes beyond providing PPE. You need to address medication safety too. Train staff on the difference between sedating and non-sedating antihistamines. Include antihistamine use in your drug policy. Make non-sedating options available through your workplace pharmacy or health program. A simple change-like stocking Claritin instead of Benadryl in the first-aid kit-can prevent a life-altering accident.The future is already here. As awareness grows, more employers will require non-sedating antihistamines for safety-sensitive roles. That’s not overreach-it’s common sense. And for the 23 million American workers who use antihistamines regularly, it could mean the difference between going home at the end of the day-or not.
Do all antihistamines make you drowsy?
No. Only first-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and hydroxyzine cause significant drowsiness because they cross into the brain. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are designed to avoid the brain and rarely cause drowsiness.
Can I drive after taking Benadryl if I don’t feel sleepy?
No. Even if you don’t feel sleepy, Benadryl impairs reaction time, coordination, and decision-making. Studies show it reduces driving performance as much as alcohol. You may feel alert, but your brain isn’t functioning normally. Never drive after taking a first-generation antihistamine.
How long does drowsiness from antihistamines last?
First-generation antihistamines can impair you for 8-18 hours after taking them, sometimes longer. Peak impairment occurs 2-4 hours after ingestion, but residual effects can linger into the next day. Second-generation antihistamines typically clear in 8-12 hours with minimal impairment.
Is it safe to take antihistamines at night if I work nights?
It’s safer to avoid first-generation antihistamines entirely if you work non-traditional hours. Even if you take them at night, they can disrupt sleep quality and cause next-day grogginess. Second-generation options are better for shift workers because they don’t interfere with alertness or sleep architecture.
Are there any antihistamines approved for pilots and commercial drivers?
Yes. The FAA and DOT prohibit first-generation antihistamines for pilots and commercial drivers. Only non-sedating options like loratadine, cetirizine, and fexofenadine are considered acceptable. Bilastine, a newer second-generation drug, is also approved in many countries for safety-sensitive roles due to its clean CNS profile.
What should I do if my doctor prescribes a sedating antihistamine?
Ask if a non-sedating alternative is available. Many doctors prescribe diphenhydramine out of habit, not because it’s the best choice. Explain your job responsibilities-whether you drive, operate machinery, or work in healthcare-and request a safer option. Most will switch you without issue.
Can antihistamines cause long-term cognitive effects?
There’s no evidence that short-term use causes permanent damage. But repeated use of sedating antihistamines can contribute to chronic fatigue, reduced productivity, and increased accident risk over time. For safety-sensitive workers, the cumulative effect is a real occupational hazard.








Bradford Beardall
January 10, 2026 AT 00:40I used to take Benadryl like candy when I was in college-thought it was just a sleep aid. Then I got hired as a forklift operator and almost ran into a rack because my hands wouldn’t stop trembling. Didn’t even realize it was the pills until my boss caught me nodding off during safety training. Now I only take Claritin. Best decision I ever made. My coworkers even ask me what’s different. I just shrug and say, ‘I stopped being a zombie.’
McCarthy Halverson
January 11, 2026 AT 03:55Second gen all the way. No debate.
Michael Marchio
January 11, 2026 AT 17:03Let’s be real here-this isn’t about safety, it’s about corporate liability. Companies don’t care if you’re impaired, they care if you get sued. That’s why they’re pushing Zyrtec and Allegra. Meanwhile, the FDA’s warning labels are still buried in 8-point font. You think this is about your brain? Nah. It’s about insurance premiums. And don’t even get me started on how pharmacies still stock Benadryl like it’s a goddamn miracle cure. It’s not. It’s a chemical nap.
Jake Kelly
January 13, 2026 AT 00:45I work night shifts at a warehouse and used to take Benadryl to help me sleep before my shift. Turns out, it made me worse. I’d zone out during inventory checks. Switched to Allegra and I’ve been sharper than ever. Didn’t even know how tired I’d been until it was gone. Good stuff.
neeraj maor
January 14, 2026 AT 02:20They’re lying. All of them. The pharmaceutical industry doesn’t want you to know that second-gen antihistamines are just repackaged first-gen with a new patent. They’re testing them on truckers in secret labs. The real danger is the P-glycoprotein nonsense-it’s a cover-up. The brain still absorbs them, just slower. And don’t get me started on how the FAA only bans them because they’re scared of lawsuits. You think they care about your safety? They care about their stock price.
Kunal Majumder
January 15, 2026 AT 21:35Bro, I’m a construction worker in Bangalore and we don’t even have access to these fancy meds. Most of us just take whatever’s cheapest. But I started asking my pharmacist for non-drowsy ones and now I bring my own. My crew noticed I’m not tripping over tools anymore. Small change, big difference.
Mario Bros
January 17, 2026 AT 02:49Just switched to Zyrtec last week and holy cow 🙌 I didn’t realize how much I was zoning out at my desk. Now I’m actually getting stuff done. My boss even asked if I got a new coffee machine. Nope. Just better meds. Life hack for the win.
Jake Nunez
January 18, 2026 AT 19:43I’m a paramedic and we used to have Benadryl in every kit. Now we stock loratadine. No more drowsy responders during 3 a.m. calls. It’s not just about me-it’s about the patient on the stretcher. If I’m slow, they pay the price.
Christine Milne
January 18, 2026 AT 20:58While I appreciate the sentiment, this article exhibits a troublingly American-centric bias. In many parts of the world, including my own country, antihistamine regulation is far more stringent, and the notion that individuals require corporate guidance to make basic pharmacological decisions is not only patronizing-it is culturally imperialistic. One does not need a Fortune 500 policy to understand that sedating drugs impair function. Basic human responsibility suffices.
Dwayne Dickson
January 20, 2026 AT 16:48Let’s contextualize this within the framework of occupational neuropharmacology. The pharmacokinetic profile of first-generation H1 antagonists-specifically their lipophilicity and lack of substrate specificity for P-glycoprotein-creates a high-risk exposure vector in safety-critical environments. The data is unequivocal. Yet, the persistent cultural normalization of diphenhydramine as a ‘sleep aid’ reflects a systemic failure in public health literacy. We are not merely discussing medication; we are addressing a cognitive dissonance epidemic.
Ted Conerly
January 22, 2026 AT 13:09I used to take Benadryl for my allergies and thought I was fine. Then I missed a deadline at work because I couldn’t focus. My wife made me switch to Claritin. I didn’t even know I was that foggy until I wasn’t. Now I’m more productive and my kids say I don’t ‘zone out’ as much during bedtime stories. Small change, huge win.
Ashlee Montgomery
January 23, 2026 AT 11:08It’s funny how we treat our brains like machines you can just plug in and turn on. We don’t think twice about taking something that slows down our thinking, then act surprised when we make mistakes. We’re not just risking our jobs-we’re risking our sense of self. If you can’t trust your own mind to be awake, what are you even doing?
Paul Bear
January 23, 2026 AT 20:57It is worth noting that the term ‘non-sedating’ is a misnomer. The FDA classifies these agents as ‘less sedating’-a critical distinction. Zero sedation is a myth. Even cetirizine, in 15% of users, induces mild drowsiness. The key is not elimination, but mitigation. And yes, the packaging has improved, but the labeling still lacks standardized, human-readable risk tiers. We need color-coded warnings-not just fine print.
lisa Bajram
January 24, 2026 AT 15:33OMG I JUST REALIZED-my entire office is on Benadryl. I swear half the people here are walking zombies. I brought in a basket of Claritin samples last week and now everyone’s asking me where I got them. I’m basically the allergy fairy 🌈✨ My boss even said I’m ‘lighting up the room’-I think he meant I’m not zoning out mid-meeting anymore. Thank you, science!
chandra tan
January 26, 2026 AT 03:16Here in India, everyone just buys whatever’s cheap. But I started reading labels and switched to fexofenadine. My cousin works on a train and said he used to fall asleep at the controls. Now he’s fine. Small change. Big life. You don’t need a PhD to read a label.