Every year, millions of people in the UK and the US reach for an OTC pill without thinking twice. A headache? Grab acetaminophen. Swollen knee? Ibuprofen from the shelf. Runny nose? A tablet of loratadine. These medications are everywhere - in kitchen drawers, gym bags, and nightstands. But just because they’re easy to buy doesn’t mean they’re safe to use without understanding them. Too many people don’t realize that acetaminophen can cause liver failure, that NSAIDs can trigger stomach bleeds, or that antihistamines can make you fall asleep behind the wheel. This isn’t about scaring you. It’s about giving you the facts so you don’t become a statistic.
NSAIDs: More Than Just Pain Relief
NSAIDs - nonsteroidal anti-inflammatory drugs - include ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin. They work by blocking enzymes that cause inflammation, pain, and fever. That’s why they’re the go-to for sprains, arthritis, and menstrual cramps. But here’s what most people miss: NSAIDs don’t just reduce pain. They also reduce your stomach’s natural protection against acid. Regular use - even just a few days a week - can lead to ulcers or dangerous internal bleeding. Studies show that people who take more than 1,200mg of ibuprofen daily have a 2.5 times higher risk of gastrointestinal bleeding.
And it’s not just your stomach. If you have high blood pressure, heart disease, or kidney problems, NSAIDs can make things worse. They can raise blood pressure, reduce kidney function, and interfere with heart medications. Even aspirin, often thought of as harmless, can cause bleeding in people taking blood thinners. If you’re over 65, or take other medications regularly, talk to a pharmacist before using NSAIDs long-term.
Topical NSAIDs like Voltaren gel (1% diclofenac) are a smarter option for joint pain. They deliver the medicine right to the sore spot with far less risk to your stomach or kidneys. For many, this is the best way to get relief without the side effects.
Acetaminophen: The Quiet Killer
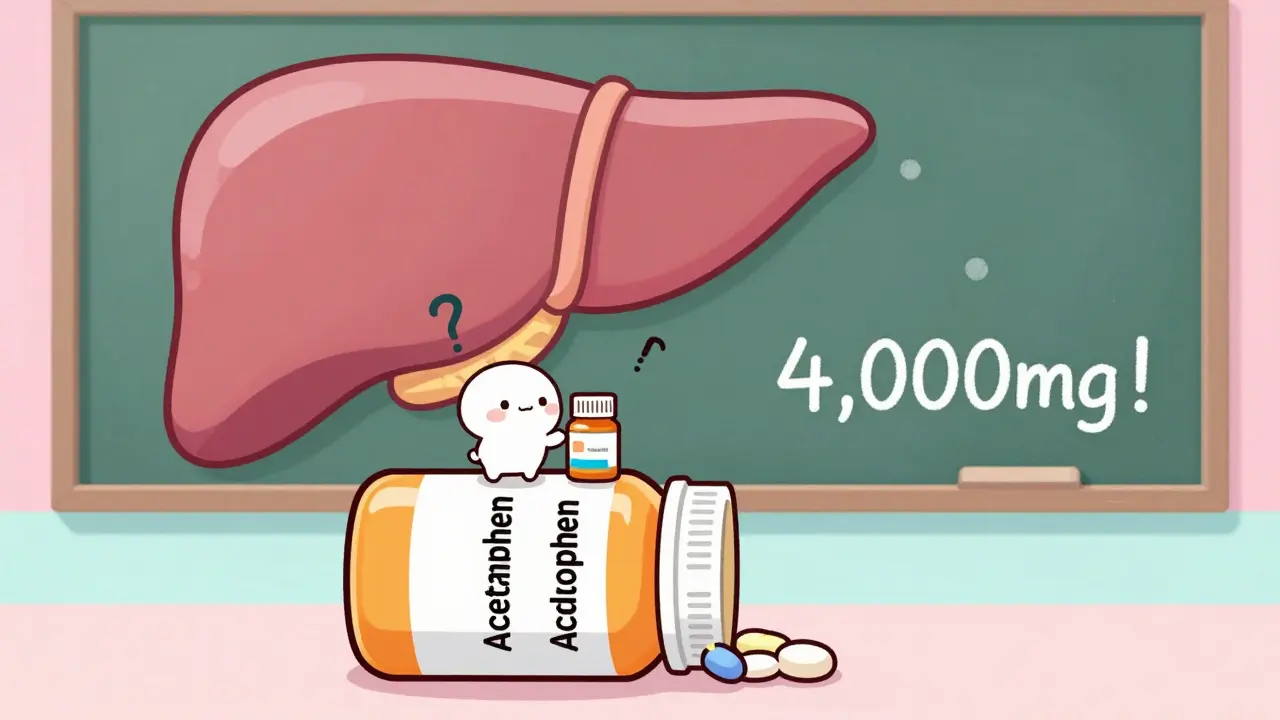
Acetaminophen (Tylenol) is the most popular painkiller in the US and the UK. Why? Because it doesn’t irritate the stomach like NSAIDs. It’s safe for people with ulcers, asthma, or bleeding disorders. But here’s the catch: it’s also the leading cause of acute liver failure in the United States. Every year, 56,000 people end up in the emergency room because they took too much - often without realizing it.
How does that happen? Simple. You take Tylenol for your headache. Later, you take a cold medicine that also contains acetaminophen. Then you take a sleep aid with it. Before you know it, you’ve hit 4,000mg - the official daily limit. But many experts now say even 3,000mg is safer. The FDA is even considering lowering the limit to 3,250mg. If you weigh less than 150 pounds, drink alcohol regularly, or have liver disease, you should never hit 3,000mg.
There’s no warning sign before liver damage kicks in. No stomach pain. No dizziness. Just fatigue, nausea, and then - sudden collapse. That’s why checking every medicine label is non-negotiable. If it says “acetaminophen,” “APAP,” or “paracetamol,” it’s the same drug. Add them all up. If you’re over the limit, stop.
Antihistamines: Sleepy vs. Non-Sleepy
Allergy season? Antihistamines are your friend. But not all are created equal. First-generation ones like diphenhydramine (Benadryl) work fast - often in 15 minutes. But they cross into your brain and cause drowsiness. In fact, half of users report feeling so sleepy they can’t drive or work safely. For older adults, this isn’t just inconvenient - it’s dangerous. A 2021 study found that seniors taking these meds had a 50% higher risk of falling.
Second-generation antihistamines - loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) - are the better choice for daily use. They don’t cross the blood-brain barrier as easily. Only about 8% of users report drowsiness. They last 24 hours, so you take one pill a day. They’re also less likely to cause dry mouth, blurred vision, or confusion.
But here’s something few know: not everyone responds the same. Some people find Zyrtec works wonders, while Claritin does nothing. That’s because of genetic differences in how your body handles histamine. If one antihistamine doesn’t help, try another. Don’t just double the dose. That won’t help - and it might hurt.
What You Should Never Do
- Don’t mix NSAIDs and acetaminophen unless you know exactly how much you’re taking. Combining them doesn’t make you feel better - it just raises your risk of liver or stomach damage.
- Don’t use OTC painkillers for more than 10 days without seeing a doctor. Persistent pain is a signal, not a nuisance.
- Don’t give adult doses to children. Liquid forms must be measured with the provided syringe or cup. A tablespoon is not a teaspoon - and 20% of pediatric overdoses happen because of this mistake.
- Don’t assume “natural” or “herbal” pain relievers are safer. Some contain hidden NSAIDs or interact dangerously with your meds.
- Don’t ignore the “Behind-the-Counter” section. Pseudoephedrine (for congestion) is kept behind the pharmacy counter. You need ID, and you’re limited to 3.6g per day. It’s not to annoy you - it’s to stop meth labs.
How to Use These Meds Safely
- Always read the Drug Facts label. It’s not filler - it’s your safety manual.
- Write down what you take and when. Use a notebook or phone app. You’d be surprised how easy it is to lose track.
- Keep all meds in their original bottles. Don’t dump pills into random containers. You might forget what’s inside.
- Store them out of reach of kids and pets. Acetaminophen is especially dangerous if a child gets into it.
- Ask your pharmacist. They’re trained to spot dangerous combinations. If you take five different meds, they can tell you which ones might clash.
- Check expiration dates. Old antihistamines lose potency. Old NSAIDs can break down into harmful chemicals.

Who Should Avoid These Meds Altogether?
- People with active ulcers or bleeding disorders - avoid NSAIDs.
- People with liver disease or who drink alcohol daily - avoid acetaminophen.
- People with asthma - avoid aspirin and other NSAIDs. They can trigger severe breathing attacks.
- People over 65 - avoid first-gen antihistamines. Use loratadine or fexofenadine instead.
- Pregnant women - acetaminophen is usually safe, but NSAIDs can harm the baby after 20 weeks.
What’s Changing in 2026?
The FDA is pushing to make OTC meds safer. In 2023, they proposed lowering the maximum daily acetaminophen dose from 4,000mg to 3,250mg. They’re also requiring clearer labeling on liquid forms - no more “TBSP” and “TSP” confusion. And in some states, even more allergy meds are moving behind the counter to prevent misuse.
Meanwhile, new topical pain gels with higher concentrations of diclofenac (3%) are hitting shelves. They’re more effective than the old 1% versions - and safer than pills. Expect more OTC transitions soon. Low-dose statins for cholesterol might be next, following the path of Prilosec.
What hasn’t changed? The fact that people still overdose because they assume OTC means “harmless.” It doesn’t. It means “available without a prescription.” That’s it.
Can I take ibuprofen and acetaminophen together?
Yes, you can take them together if you need stronger pain relief - but only if you stay within the daily limits for each. For example: 600mg ibuprofen every 8 hours (max 1,800mg/day) and 650mg acetaminophen every 8 hours (max 2,000mg/day). Never exceed 3,000mg of acetaminophen total. Always space doses apart and avoid combining them with other products that contain either drug.
Is one antihistamine better than another?
It depends on your body. Loratadine (Claritin) and fexofenadine (Allegra) are least likely to cause drowsiness. Cetirizine (Zyrtec) works faster and stronger for some people but causes mild sleepiness in about 15% of users. If one doesn’t help after 3 days, try another. Don’t double the dose. Genetic differences mean your body responds uniquely to each drug.
Why do some OTC meds have lower doses than prescription versions?
Because OTC drugs are meant for short-term, self-managed use. For example, Prilosec OTC is 20mg, while the prescription version is 40mg. This reduces the risk of long-term side effects like nutrient deficiencies or bone loss. It’s not about being weaker - it’s about being safer for people who don’t have a doctor guiding them.
Can I drink alcohol while taking acetaminophen?
No. Even one drink with acetaminophen increases liver damage risk. If you drink regularly - even just a glass of wine a night - you should avoid acetaminophen entirely. Your liver processes both substances the same way. Together, they overwhelm it. The damage can be silent until it’s too late.
What should I do if I think I’ve taken too much?
Call emergency services or poison control immediately - don’t wait for symptoms. Acetaminophen overdose can take 12-24 hours to show signs, but treatment is most effective within 8 hours. For NSAIDs, symptoms like vomiting, dizziness, or ringing in the ears mean you’ve exceeded safe levels. Go to the ER. Don’t try to “wait it out.”
Final Advice: Know Your Dose
OTC meds are powerful tools - not toys. They’ve saved millions from pain and discomfort. But they’ve also sent thousands to the hospital because people didn’t know what they were taking. The key isn’t avoiding them. It’s knowing how to use them. Read the label. Track your doses. Talk to your pharmacist. If you’re unsure, don’t guess. Your body will thank you.







Bobbi-Marie Nova
January 15, 2026 AT 22:33Finally someone who gets it. I used to pile up Tylenol and Advil like candy until my liver enzymes went haywire. Now I keep a little notebook. One pill at a time. No more guessing.
Riya Katyal
January 16, 2026 AT 11:53Oh wow, so you’re saying I shouldn’t take Benadryl before my Zoom meetings? Who knew? Maybe next you’ll tell me water isn’t technically a drug.
swarnima singh
January 16, 2026 AT 18:33i just took 2 tylenol for my head ache and then a cold med because i was sneezing... now im scared. like, what if i already ruined my liver? i dont even know what apap means. why do they make it so confusing? i just wanted to feel better.
kanchan tiwari
January 17, 2026 AT 13:34THEY KNOW. They know we’re popping pills like Skittles. That’s why the labels are so tiny. That’s why they hide APAP in 17 different products. This isn’t about safety-it’s about profit. Big Pharma wants you addicted to the shelf, not the doctor. They’re counting on your ignorance.
And don’t even get me started on how they let diclofenac gel become OTC but kept pseudoephedrine behind the counter. One helps your knee, the other helps someone cook crystal meth. Which one do you think makes more money?
They don’t want you smart. They want you numb. And if you’re numb enough, you’ll keep buying.
I’m not paranoid. I’ve read the FDA documents. The warnings are there. They’re just buried under 14 layers of legalese and glittery branding.
john Mccoskey
January 19, 2026 AT 10:04The data is clear, and yet the public remains willfully obtuse. NSAIDs inhibit COX-1 and COX-2 enzymes, which reduces prostaglandins responsible for inflammation-but also those that maintain gastric mucosal integrity. The risk of GI bleeding increases exponentially with chronic use, particularly in those over 60, with H. pylori infection, or on anticoagulants. The 2.5x multiplier cited isn’t an outlier-it’s replicated across multiple cohort studies, including the British Medical Journal’s 2020 meta-analysis.
Meanwhile, acetaminophen’s hepatotoxicity is mediated by NAPQI accumulation when glutathione reserves are depleted. Alcohol consumption reduces glutathione synthesis, which is why even moderate drinking with daily acetaminophen creates a synergistic risk profile that’s clinically documented. The FDA’s proposed reduction to 3,250mg isn’t conservative-it’s overdue.
And antihistamines? First-gen H1 blockers like diphenhydramine cross the blood-brain barrier because they’re lipophilic and uncharged at physiological pH. Second-gen agents like fexofenadine are zwitterionic, limiting CNS penetration. This isn’t marketing-it’s pharmacokinetics. But most consumers don’t care. They want fast relief. They don’t want to understand why.
What’s truly tragic is that pharmacists are trained to catch these interactions, yet most patients don’t even ask. They assume the shelf is safe. It’s not. It’s a minefield disguised as convenience.
And don’t get me started on the ‘natural’ supplements. Turmeric extract with undisclosed NSAID analogs? Yes, it’s real. The FDA has issued 47 warning letters in the last 18 months alone to companies selling ‘herbal pain relievers’ laced with diclofenac or celecoxib. People think they’re being clever by avoiding pharmaceuticals. They’re just poisoning themselves with a side of virtue signaling.
Education isn’t optional. It’s the only thing standing between a healthy population and a generation of iatrogenic liver failures, GI bleeds, and accidental overdoses. And until people treat OTC meds like actual medicine-not candy-the death toll will keep rising.
Joie Cregin
January 20, 2026 AT 00:23I used to take Zyrtec like it was gum-until I realized I was nodding off at my desk. Switched to Allegra. No drowsiness. No drama. Just quiet relief. It’s wild how one tiny change made my whole life less foggy.
Also, I keep all my meds in the original bottles now. My cat almost ate a bottle labeled ‘Migraine Relief’ that turned out to be naproxen. She’s fine. But I nearly had a heart attack.
Pharmacists are heroes. Talk to them. They know more than Google.
Ryan Hutchison
January 20, 2026 AT 05:54America’s biggest problem isn’t the meds-it’s the people who think they know better than science. You want to take ibuprofen with a beer? Go ahead. But don’t come crying when your stomach starts bleeding. This isn’t a suggestion. It’s biology.
And for the love of God, stop mixing OTC drugs like you’re cooking a stew. Read the label. It’s not hard. It’s written in English. Not Mandarin. Not hieroglyphs. ENGLISH.
We don’t need more regulations. We need more common sense. And apparently, that’s in short supply.
Bianca Leonhardt
January 21, 2026 AT 03:34You think this is bad? Wait till you see what’s coming next. They’re going to make melatonin OTC. And then people will be taking 10mg a night and wondering why they’re hallucinating. It’s not a vitamin. It’s a hormone. And you’re treating it like sugar.
Everyone’s so focused on acetaminophen and NSAIDs, but no one’s talking about how many people are now on 3 different antihistamines at once because ‘one didn’t work.’
It’s not ignorance. It’s arrogance. And it’s killing people.
waneta rozwan
January 21, 2026 AT 07:09My grandma took Tylenol every day for her ‘aches’ and ended up in the hospital with liver failure. She didn’t even know her cold medicine had it too. She thought ‘natural’ meant safe. She died because she trusted the label and didn’t read it.
I keep a little card in my wallet now. List of meds. Dosages. Times. I don’t trust my brain anymore. And I’m only 32.
Nicholas Gabriel
January 22, 2026 AT 13:30Just a quick note: if you’re taking more than one OTC product, please, please, PLEASE write it down. I used to be the guy who’d take Advil for the knee, NyQuil for the cold, and Excedrin for the headache-thinking I was being proactive. Turns out, I was just giving my liver a three-course meal of toxins.
Now I use a free app called MedTracker. It alerts me if I’m overlapping ingredients. I didn’t even know that “APAP” was acetaminophen until I started using it. I’m not a doctor. I’m not a pharmacist. I’m just someone who didn’t want to end up in the ER.
If you’re reading this and you’ve ever taken two OTC meds on the same day… stop. Just stop. Look at the labels. Add them up. You might be surprised.
And if you’re over 65? Please, for the love of everything holy, avoid Benadryl. There are better options. Your brain will thank you.
Henry Ip
January 23, 2026 AT 08:45One thing I learned the hard way-don’t assume your body handles meds the same as your friend’s. I took Zyrtec and felt fine. My sister took it and couldn’t stand up. We’re both 35, same weight, same diet. Genetics. It’s real. Try another if one doesn’t work. Don’t double up. It doesn’t help. It just hurts.
And yes, talk to your pharmacist. They’re not just the people who hand you the box. They’re the ones who catch the dangerous combos before you even walk out the door.
Cheryl Griffith
January 23, 2026 AT 22:23I used to think OTC meant ‘safe for everyone.’ Then I watched my dad take ibuprofen every day for his back and end up with a bleeding ulcer. He didn’t have symptoms until he passed out at the grocery store.
Now I check every label like it’s a bomb defusal manual. APAP? That’s acetaminophen. Ibuprofen? That’s NSAID. No mixing unless I’ve counted it all out.
It’s not paranoia. It’s survival.
Isabella Reid
January 24, 2026 AT 05:26I’m from India, and I’ve seen people here take three different painkillers at once because ‘it works faster.’ No one checks labels. No one asks. They trust the shopkeeper. And sometimes, the shopkeeper doesn’t even know what’s in the pill.
It’s terrifying. But I’m trying to change it. I keep a printed list of what each OTC drug does in Hindi and English. I hand it out at the market. One person at a time.
Knowledge isn’t power. It’s protection.
brooke wright
January 24, 2026 AT 20:17My 12-year-old cousin took a whole bottle of children’s Tylenol thinking it was candy. She’s fine now. But the ER nurse said if it had been just one more hour, she might not have made it. Don’t ever assume your kid knows what’s safe.
Lock your meds. Like, actually lock them. Not just put them on the top shelf. A locked box. A cabinet with a latch. Your kid is smarter than you think.
john Mccoskey
January 26, 2026 AT 16:43That last comment about the child? That’s the quiet horror most people never consider. The real tragedy isn’t the adults who self-medicate recklessly-it’s the kids who don’t know any better. And the adults who let them have access. You think a locked cabinet is overkill? It’s not. It’s the difference between a hospital visit and a funeral.