Liquid Medicine Safety: How to Store, Use, and Avoid Dangerous Mistakes
When you’re giving liquid medicine, a form of medication designed for easy swallowing, often used for children, elderly patients, or those with trouble swallowing pills. Also known as oral suspensions, it’s one of the most common ways people take drugs—but also one of the most error-prone. A wrong dose, bad storage, or confusing label can turn a helpful treatment into a serious risk. Unlike pills, liquid medicines don’t come in fixed amounts. You’re measuring with cups, syringes, or droppers—and that’s where things go wrong.
Medication storage, how and where you keep your drugs to maintain their strength and safety. Also known as pharmaceutical storage, it’s not just about keeping them out of reach of kids. Heat, light, and moisture can destroy liquid medicines fast. A bottle of amoxicillin suspension might last 14 days in the fridge but only 7 days at room temperature. Keep it cold? Good. Leave it on the bathroom counter? That’s how you end up with a useless, maybe even harmful, dose. Same goes for insulin, seizure meds, or antibiotics—each has its own rules. And don’t assume your pharmacist told you everything. If you’re not sure, ask: "What happens if this sits in the sun?"
Drug interactions, when one medicine changes how another works in your body. Also known as medication interactions, they’re especially dangerous with liquids because they’re often mixed with food, juice, or other meds. A child on antibiotics might get less relief if the liquid is mixed with orange juice—citric acid can break down the drug. An elderly person taking a blood thinner might face bleeding risks if their liquid painkiller contains alcohol. Even something as simple as giving a child liquid Tylenol and a cold syrup at the same time can lead to double dosing. You’re not just giving medicine—you’re managing a chemical system inside the body.
Pediatric dosing, the precise calculation of liquid medicine amounts for children based on weight and age. Also known as child-specific medication dosing, it’s not a guess. A teaspoon isn’t a teaspoon. A kitchen spoon holds more than a medical dosing cup. The wrong amount can be deadly—too little and the infection spreads; too much and the liver gets damaged. That’s why every liquid medicine for kids comes with a dosing tool. Use it. Don’t improvise. And never, ever use an old bottle’s dropper for a new prescription. Labels change. Concentrations change. What worked last month might be five times stronger this month.
And then there’s medicine labeling, clear, accurate, and consistent information on the bottle that tells you what’s inside, how much to take, and when. Also known as pharmaceutical labeling, it’s your last line of defense. Is the label faded? Is the concentration listed in mg/mL? Is there an expiration date? Many people miss that the same drug can come in different strengths—like 125mg/5mL versus 250mg/5mL. One mistake, one misread number, and you’re giving a full adult dose to a toddler. That’s not hypothetical. That’s in the emergency room records.
You won’t find all these details on a pharmacy sticker. You won’t see them in a 30-second doctor’s visit. But you’ll find them here—in real stories, real data, and real mistakes that happened to real people. From how to safely store liquid antibiotics while traveling, to why some meds must never be mixed with milk, to how to read a label when the print is too small—this collection gives you what no pharmacist has time to explain. You’re not just reading about safety. You’re learning how to stop a preventable accident before it happens.
How to Confirm Pediatric Dosing on a Child’s Prescription Label
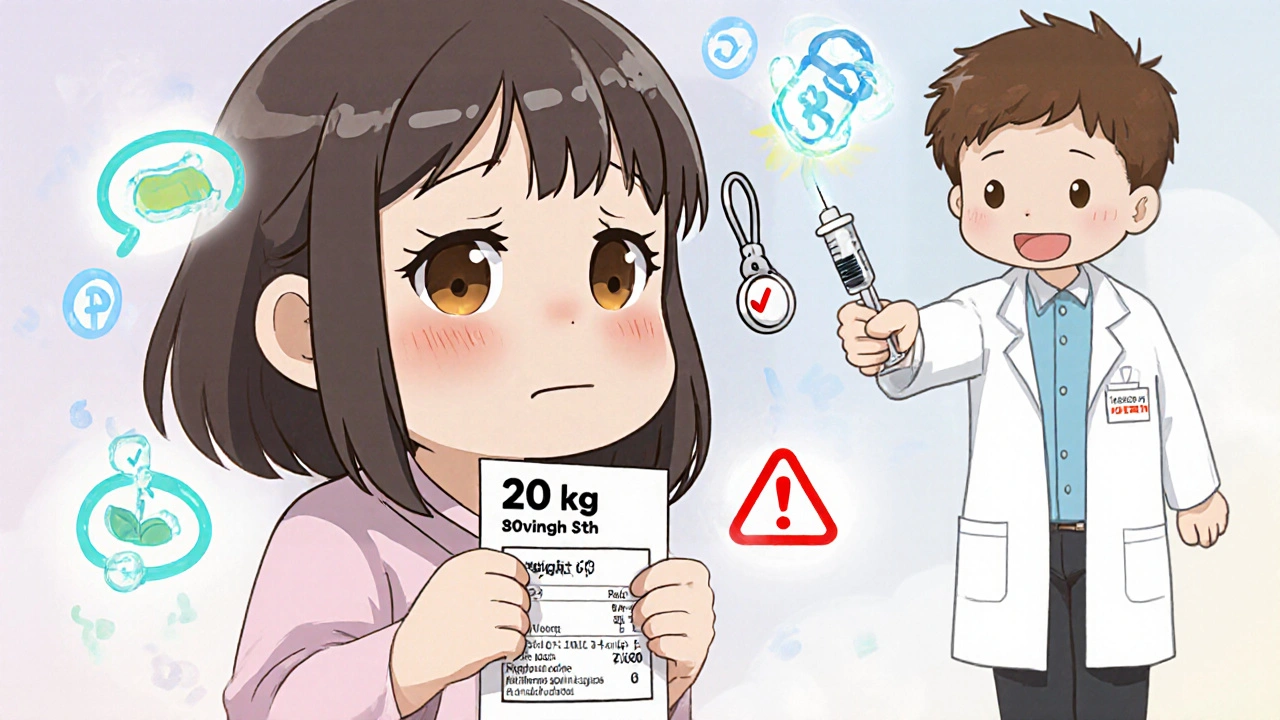
Learn how to confirm your child's medication dose by checking weight in kilograms, verifying milligrams (not milliliters), and asking key questions at the pharmacy. Prevent dangerous dosing errors with simple, proven steps.
read more



