Overdose recognition can mean the difference between life and death when a loved one is in danger. In 2022, over 107,000 Americans died from drug overdoses-most happening at home. Family members often spot the first signs, but without proper training, they might miss them. This guide breaks down exactly what to look for and how to respond.
According to CDCthe Centers for Disease Control and Prevention data, 78% of overdose deaths occur in private residences. That means when someone overdoses, family members or roommates are usually the first on the scene. Research from the Journal of Addiction Medicine shows that immediate action by bystanders can reduce overdose deaths by up to 40%. But recognizing the symptoms isn’t always obvious-especially with different drugs like opioids versus stimulants.
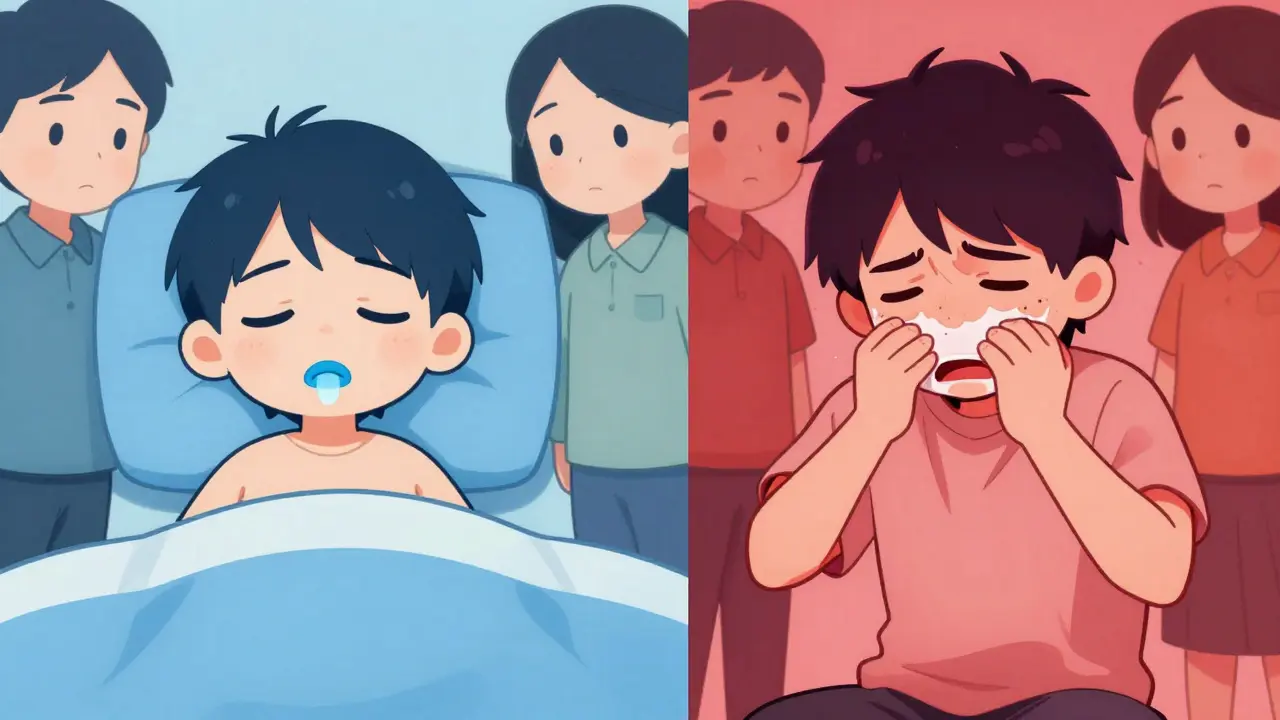
Spotting Opioid Overdose Symptoms
The opioid triada set of three key signs indicating opioid overdose is the core set of signs for opioid overdoses (like heroin, fentanyl, or prescription painkillers). First, check for unresponsiveness. Shout their name or rub their sternum firmly-if they don’t react, that’s a red flag. Second, look at their breathing. Fewer than one breath every five seconds or no breathing at all indicates respiratory depressionabnormally slow or shallow breathing. Third, check their lips and nails for cyanosisbluish or ashen discoloration from lack of oxygen-a blue or purple tint. On darker skin tones, this might appear as grayish or ashen instead of blue.
Other signs include clammy skin, limp body posture, and gurgling sounds. These often happen together. For example, a person might be unresponsive, with shallow breathing and a bluish tint around the mouth. Remember: if they don’t respond to physical stimulation (like a sternum rub), it’s likely an overdose, not just being high.
Recognizing Stimulant Overdoses
Stimulant overdoses (from cocaine, methamphetamine, or prescription ADHD meds) look very different. Instead of slow breathing, you’ll see rapid heartbeat, high fever (over 104°F), seizures, or chest pain. The person might be extremely agitated, sweating heavily, or having muscle spasms. Unlike opioids, they might be conscious but in distress. For example, a friend who’s shaking uncontrollably with a racing heart could be experiencing a cocaine overdose. Always call 911 immediately-stimulant overdoses can cause heart attacks or strokes quickly.
What to Do When You Spot an Overdose
Time is critical. Here’s what to do right away:
- Call 911 immediately. Say "drug overdose" so responders know it’s urgent.
- If the person isn’t breathing, start CPR (chest compressions at 100-120 per minute).
- Administer naloxonea medication that reverses opioid overdoses if available. For nasal spray, insert the nozzle into one nostril and press the plunger. For injection, give it into the thigh muscle.
- Wait 2-3 minutes. If they don’t wake up, give a second dose.
- Stay with them until help arrives. Even if they wake up, they still need medical care.

How to Train Family Members Effectively
Studies show that hands-on practice makes training stick. The CDC found that programs using real training naloxone kits and scenario-based drills have 89% skill retention after three months-compared to just 42% for lecture-only sessions. Dr. Nora Volkow of NIDAthe National Institute on Drug Abuse says families retain 73% more information when practicing realistic scenarios.
Here’s how to train:
- Use a training naloxone kit (they’re cheap and safe-no actual drug).
- Practice on mannequins or each other to simulate real-life steps.
- Review scenario cards: "What would you do if someone is unresponsive with slow breathing?"
- Discuss skin tone differences-practice identifying cyanosis on various skin shades.
Overcoming Common Challenges
Many families hesitate to train because they fear "jinxing" their loved one or feel overwhelmed. But 92% of those who trained later said the fear faded after practice. The Georgia Coastal Health District trained 1,247 family members, and 87 of them used their skills to save lives-94% survived. Language barriers are another issue. SAMHSASubstance Abuse and Mental Health Services Administration offers training materials in 28 languages, and many community groups provide translators during sessions. If you’re unsure where to start, the Overdose Lifelinea harm reduction organization providing overdose education app (free to download) has step-by-step videos and practice tools.
Can naloxone be used for any drug overdose?
No, naloxone only works for opioid overdoses (like heroin, fentanyl, or prescription painkillers). It won’t help with stimulant overdoses (cocaine, meth) or alcohol poisoning. Always call 911 first-medical professionals can handle other types of overdoses.
Is it safe to use naloxone if I’m not sure it’s an opioid overdose?
Yes. Naloxone is safe to use even if it’s not an opioid overdose. It has no effect on non-opioid substances and won’t harm someone who isn’t overdosing. The CDC recommends administering it immediately if you suspect an opioid overdose.
Where can I get naloxone training?
Many pharmacies offer free naloxone training with purchase. Community health centers, harm reduction groups, and local health departments also provide free sessions. The Overdose Lifeline app includes step-by-step video instructions. In 31 states, you can get naloxone without a prescription through standing orders.
What should I do if the person wakes up after naloxone?
Even if they wake up, they still need medical care. Naloxone wears off in 30-90 minutes, and the overdose could return. Stay with them until EMS arrives. Keep them calm and monitor their breathing.
Can I be held legally responsible if I help someone overdose?
Most states have Good Samaritan laws that protect people who help in overdose situations. These laws prevent legal action for calling 911 or administering naloxone. Check your state’s specific laws, but generally, helping is encouraged and protected.
Should I perform CPR before or after giving naloxone?
If the person isn’t breathing, start CPR immediately while someone else calls 911. If you’re alone, do 2 minutes of CPR (about 100 compressions) before calling 911. Then administer naloxone as soon as possible. CPR keeps oxygen flowing until help arrives.
Are there different signs for fentanyl overdoses?
Fentanyl overdoses look like other opioid overdoses but often happen faster. The opioid triad applies: unresponsiveness, slow breathing, cyanosis. However, fentanyl is so potent that symptoms can develop within minutes. Always treat it as a medical emergency-call 911 and use naloxone immediately.
Can I train my family members if I’ve never dealt with an overdose before?
Yes. Many training programs are designed for beginners. Start with free online resources like the Overdose Lifeline app or SAMHSA’s guides. Practice with a training kit. You don’t need prior experience-just willingness to learn. Most family members say training was easier than they expected.
Is it true that overdoses can happen with prescription drugs?
Yes. Prescription opioids like oxycodone or fentanyl patches can cause overdoses, especially if misused. Always store them safely, and teach family members the overdose signs. Naloxone works for prescription opioid overdoses too.
Where can I find local overdose prevention training?
Check your state health department website, local harm reduction organizations, or pharmacies. Many offer free in-person or virtual sessions. The National Harm Reduction Technical Assistance Center has a directory of training providers nationwide.







Georgeana Chantie
February 6, 2026 AT 17:15Parents shouldn't have to deal with overdose emergencies. That's what hospitals are for. 🤷♀️
Jennifer Aronson
February 7, 2026 AT 15:17According to CDC data, 78% of overdose deaths occur in private residences. Immediate action by bystanders can reduce deaths by up to 40%. Family training is essential for timely response.
Arjun Paul
February 9, 2026 AT 03:34This data is outdated. Current studies show higher hospital rates. Training families is ineffective. They'll just panic.
Nancy Maneely
February 10, 2026 AT 23:55This guide is way too basix. Real life overdoses are way more complex. Like, seriously, who even uses this? 😭
Phoebe Norman
February 12, 2026 AT 03:28Naloxone is specific to opioid receptor antagonism Non-opioid overdoses require alternative interventions Immediate medical attention is non-negotiable No margin for error
Kate Gile
February 12, 2026 AT 20:31Training families is vital! Hands-on practice with naloxone kits makes a huge difference. Let's get everyone involved. 💪
Gregory Rodriguez
February 14, 2026 AT 09:21Okay, let's get real for a second.
This guide is actually pretty spot-on, which is rare for these kinds of things.
Most people think overdoses are only for junkies, but the truth is, it can happen to anyone-your grandma with pain meds, your cousin with ADHD meds, even your buddy who thinks they're "just partying."
The opioid triad is spot-on: unresponsive, slow breathing, blue lips.
But for stimulants? It's a whole different beast-seizures, chest pain, fever.
And naloxone? Only works for opioids, so don't waste time trying it on cocaine or meth.
But the real kicker? Practicing with training kits makes all the difference.
I did a hands-on session last month, and honestly, it was way easier than I thought.
Like, inserting the nasal spray? Simple.
Doing chest compressions? Just follow the beat of Stayin' Alive.
The CDC says 89% retention after three months with hands-on training-that's huge!
Most people think they can't do it, but the truth is, anyone can learn this stuff.
So yeah, maybe it's a bit basic, but it's also life-saving.
Let's not overcomplicate it.
Just learn the basics, keep naloxone handy, and call 911.
That's it. Simple. Effective. Life-saving.
Seriously, why wouldn't you want to know this? 🤷♂️
divya shetty
February 14, 2026 AT 19:36It is imperative that all family members undergo comprehensive training. Failure to do so is a dereliction of duty. The consequences are severe.
anjar maike
February 16, 2026 AT 13:29Naloxone is lifesaving 🌟 Just practice with training kits