Medication Errors: What They Are, How They Happen, and How to Prevent Them
When you take a pill, apply a cream, or get an injection, you expect it to help—not hurt. But medication errors, mistakes in prescribing, dispensing, or taking drugs that lead to harm. Also known as drug errors, these aren’t just rare accidents—they’re a leading cause of preventable injury in hospitals and homes alike. A study from the National Academy of Medicine found that the average American patient is exposed to at least one medication error per year. That’s not a glitch. That’s a system problem.
These errors don’t just happen because someone misreads a handwriting. They come from overlapping gaps: a doctor prescribing the wrong dose because they didn’t check a patient’s kidney function, a pharmacist filling the right drug but the wrong strength, a nurse giving it at the wrong time, or a patient mixing their blood thinner with grapefruit juice because no one explained the risk. adverse drug events, harmful outcomes directly caused by medication use. Also known as drug reactions, these are often the end result of a chain of small mistakes. And it’s not just older adults. Kids, pregnant women, people on five or more meds—they’re all at risk. Women, for example, are twice as likely to have bad reactions to certain drugs, not because they’re more sensitive, but because most clinical trials still use male bodies as the default.
prescription errors, mistakes made when a doctor writes or electronically sends a drug order. Also known as prescribing mistakes, these include wrong drug, wrong dose, wrong patient, or no allergy check. They’re behind half of all medication errors. And then there’s the pharmacy side—dispensing errors, giving the patient the wrong medication or incorrect instructions. Also known as filling mistakes, these can happen when labels get mixed up or when a busy pharmacist misses a drug interaction. Even something as simple as confusing "QD" (once daily) with "QID" (four times daily) can land someone in the ER.
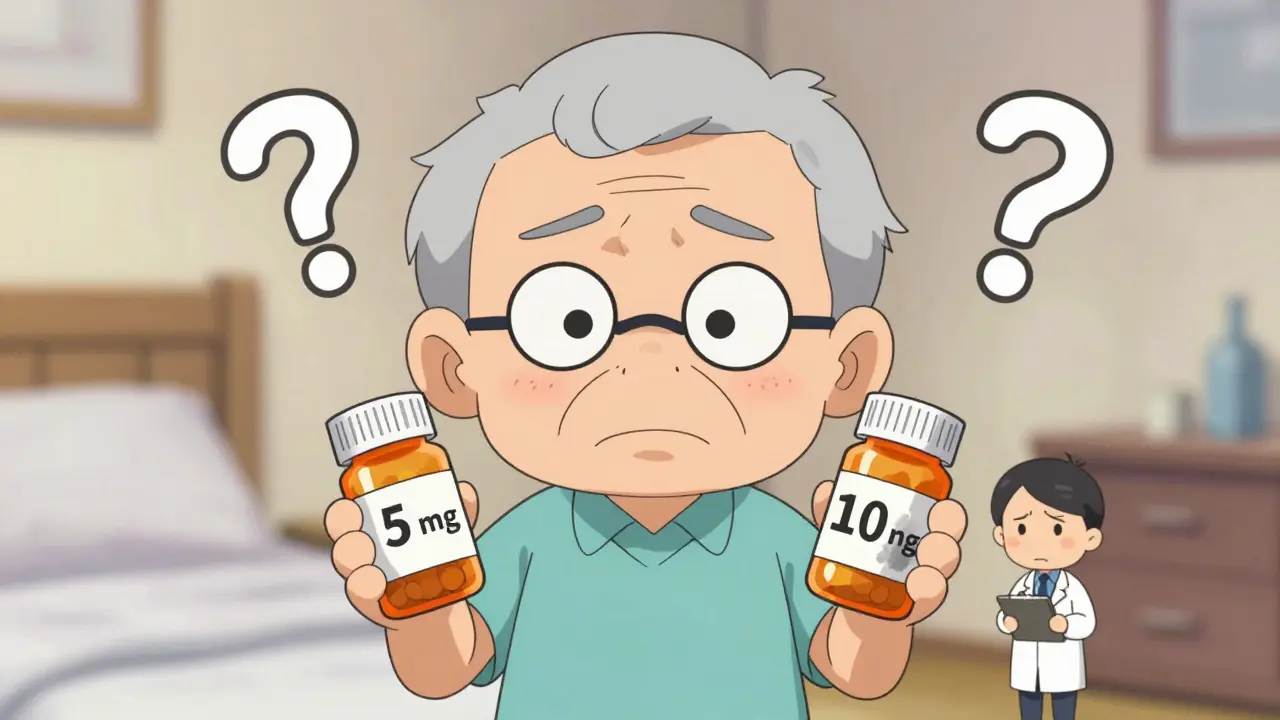
You might think, "I’m careful. I read the label." But labels change. New generics hit the market. Pills look different. And if you’re juggling six meds for high blood pressure, diabetes, arthritis, and depression, it’s easy to mix them up. That’s why the best defense isn’t just vigilance—it’s communication. Always ask: "What’s this for?" "What happens if I miss a dose?" "Could this interact with my other meds?" And if you’re helping a parent or elderly relative, don’t assume they understand the instructions. Write them down. Use a pill organizer. Take a photo of the prescription label.
What you’ll find in the articles below isn’t just a list of drugs. It’s a map of where things go wrong—and how to fix them. From nasal sprays that cause drowsiness if misused, to blood thinners that need strict monitoring, to antifungals that can interact with heart meds—each post shows how real people got caught in the gaps. You’ll see how gender affects side effects, how online pharmacies can help—or hurt, and how even something as simple as magnesium hydroxide can cause trouble if taken with the wrong other pills. This isn’t about fear. It’s about power. The power to ask the right questions, spot red flags, and protect yourself before the error happens.
Medication Errors vs Drug Side Effects: How to Tell Them Apart and Why It Matters
Learn how to tell the difference between preventable medication errors and unavoidable drug side effects. Knowing this can help you avoid harm and push for safer care.
read moreHow to Reconcile Medications After Hospital Discharge to Avoid Dangerous Interactions

After hospital discharge, medication errors cause thousands of preventable readmissions. Learn how to reconcile your meds step by step to avoid dangerous drug interactions and stay safe at home.
read moreCost-Saving Strategies While Maintaining Medication Safety

Discover how hospitals and patients can cut medication costs without risking safety-through pharmacist-led care, generics, better communication, and smart tech use. Real data, real savings.
read more